Assessment |
Biopsychology |
Comparative |
Cognitive |
Developmental |
Language |
Individual differences |
Personality |
Philosophy |
Social |
Methods |
Statistics |
Clinical |
Educational |
Industrial |
Professional items |
World psychology |
Clinical: Approaches · Group therapy · Techniques · Types of problem · Areas of specialism · Taxonomies · Therapeutic issues · Modes of delivery · Model translation project · Personal experiences ·
Wartenberg's migratory sensory neuropathy (also known as Wartenberg's migrant sensory neuritis) (WMSN) is a rare form of neuropathy identified by Robert Wartenberg in 1958 which is easy to confuse with the early stages of multiple sclerosis or Guillain-Barré syndrome. However this is a benign relapsing and remitting condition in which pain and subsequent loss of sensation in the distribution of individual cutaneous nerves is induced by movement of the limbs inducing stretch.[1] The movements may be very small, and the periods of pain, dysaesthesia, and numbness can vary from almost instantaneous to chronic. In some cases, reports discount WMSN as a diagnosis where there is less prominent pain.[2] Wartenberg’s sensory neuritis is a distinct, exclusively sensory, neuropathy, marked by pain preceding numbness in affected nerves. An episode of stretching preceding pain is not necessary for the diagnosis. Wartenberg’s sensory neuritis often retains its spotty, exclusively sensory characteristics after long term follow-up.[3]
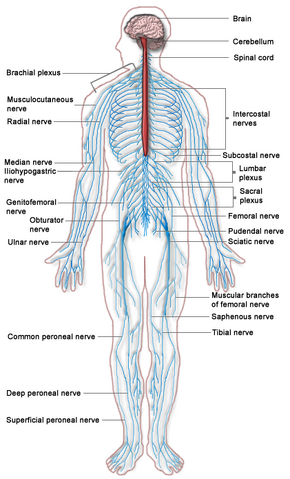
The Human Nervous System. Blue is PNS while red is CNS.
Only a few case studies have ever been reported,[4] and even of Wartenberg's own patients only 2 of the 9 conform strictly to his own description of the clinical characteristics; however there are a couple of surprising case clusters of this condition in both the Thames Valley and San Francisco.[5]The limited number of published clinical studies seems to suggest that it is a rare disorder. Most studies included few patients and were retrospective.[6]
Cause[]
While the actual cause of this polyneuropathy remains unknown, most research now puts this as an immune-mediated, chronic, asymmetric polyneuropathy.[7][8] Stress may also be a contributory factor.
Symptoms[]
Positive Tinel's sign is often present.[9] Any cutaneous sensory nerve can be involved with patients usually showing a slow start, building up to sensations in many parts of the body.[10] At times, the focal nerve lesions can be painful. Most symptoms resolve but permanent sensory loss can persist. Electrodiagnostic studies demonstrate axon loss in the distribution of the involved cutaneous nerves [1]. Patients sometimes described a sensation of electric discharge when elongating nerve trunks. In half of the cases the attacks of dysesthesia or of sensory loss followed one another within less than one year. The deficits were fully reversible in a third of the cases studied by Rev Neurol (Paris) after a mean total evolution of 4 to 8 years.
Mean onset age, 35 years with a range of 4th and 5th decades.[11][12]
Pure sensory mononeuritis multiplex
Course: Episodic; Recurrent Some sensory loss improves, Other is permanent
Sensory loss: Discrete areas: Involvement of individual cutaneous nerves Sudden onset
Distribution: Legs; Arms; Trunk; Face
Pain:In areas of sensory loss
Painful dysesthesias: Induced by limb stretch or movement
Electrodiagnostic: Multifocal axon loss
Pathology: Biopsy of affected nerve in typical cases with a clinical history and neurological and electrophysiological findings consistent with Wartenberg’s sensory neuritis, a nerve biopsy can reasonably be omitted from the diagnostic work-up
Perineurial scarring Chronic inflammation
Axonal loss & regeneration: Differential fascicular involvement
Endoneurial edema Immunoglobulin deposition
Treatments[]
Due to the unknown cause of this condition, treatment seems to be symptomatic and individual to the patient. Steroid treatments such as prednisone don't seem to work[8] but there is anecdotal evidence for the use of amitriptyline, and either pregabalin or gabapentin[13] along with a variety of painkillers. This is often treated similarly to diabetic neuropathic pain, but diabetes is not necessarily present.
Wartenberg's Syndrome[]
WMSN is not to be confused with Wartenberg's syndrome - a radial sensory nerve entrapment causing significant pain in the lower 1/3 of the forearm.[14]
References[]
- ↑ Matthews WB, Esiri M (Jan 1983). The migrant sensory neuritis of Wartenberg. J Neurol Neurosurg Psychiatr. 46 (1): 1–4.
- ↑ http://www.elsevier-international.com/e-books/viewbook.cfm?ID=942
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2910306/
- ↑ Zifko UA, Hahn AF (1997). Migrant sensory neuropathy: report of 5 cases and review of the literature. J Peripher Nerv Syst. 2 (3): 244–9.
- ↑ Hudgson P (Sep 1983). The migrant sensory neuritis of Wartenberg. Br Med J (Clin Res Ed) 287 (6394): 704.
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2910306/
- ↑ http://www.avondalemedical.com/pdf_files/PNMar2005/PN0305FeaNeuropathy.pdf
- ↑ 8.0 8.1 Nicolle MW, Barron JR, Watson BV, Hammond RR, Miller TA (Mar 2001). Wartenberg's migrant sensory neuritis. Muscle Nerve 24 (3): 438–43.
- ↑ Laterre C, Ghilain S, Tassin S, Guérit JM (1988). [Wartenberg's disseminated sensory neuropathy]. Rev Neurol. (Paris) 144 (5): 358–64.
- ↑ Hamano T, Kaji R, Oka N, Akiguchi I, Kimura J (Oct 1992). [Migrant sensory neuritis—electrophysiological and pathological study]. Rinsho Shinkeigaku 32 (10): 1112–6.
- ↑ http://neuromuscular.wustl.edu/nanatomy/asymmetric.html#wartenberg
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2910306/
- ↑ http://www.partialobserver.com/Wartenberg.cfm#id35
- ↑ http://www.whonamedit.com/synd.cfm/1979.html Who Named it? website
| This page uses Creative Commons Licensed content from Wikipedia (view authors). |