Assessment |
Biopsychology |
Comparative |
Cognitive |
Developmental |
Language |
Individual differences |
Personality |
Philosophy |
Social |
Methods |
Statistics |
Clinical |
Educational |
Industrial |
Professional items |
World psychology |
Biological: Behavioural genetics · Evolutionary psychology · Neuroanatomy · Neurochemistry · Neuroendocrinology · Neuroscience · Psychoneuroimmunology · Physiological Psychology · Psychopharmacology (Index, Outline)
| ICD-10 | E750 | |
|---|---|---|
| ICD-9 | 330.1 | |
| OMIM | 268800 | |
| DiseasesDB | 29469 | |
| MedlinePlus | [1] | |
| eMedicine | / | |
| MeSH | {{{MeshNumber}}} | |
Sandhoff disease is a rare inherited lipid storage disorder that causes progressive destruction of nerve cells in the brain and spinal cord.
History[]
Sandhoff disease was first illustrated in Life Science in 1968 by a German chemist named Konrad Sandhoff. Konrad Sandhoff investigates biochemical and enzymatic aspects of the gangliosidoses and other storage diseases.
Types[]
The most common and severe form of Sandhoff disease begins in infancy. Infants with this disorder typically appear normal until the age of 3 to 6 months, when development slows and muscles used for movement weaken. Affected infants lose motor skills such as turning over, sitting, and crawling. As the disease progresses, infants develop seizures, vision and hearing loss, mental retardation, and paralysis. An eye abnormality called a cherry-red spot, which can be identified with an eye examination, is characteristic of this disorder. Some infants with Sandhoff disease may also have enlarged organs (organomegaly) or bone abnormalities. Children with the severe form of this disorder usually live only into early childhood.
Other forms of Sandhoff disease are very rare. Signs and symptoms can begin in childhood, adolescence, or adulthood and are usually milder than those seen with the infantile form of Sandhoff disease. As in the infantile form, mental abilities and coordination are affected. Characteristic features include muscle weakness, loss of muscle coordination (ataxia) and other problems with movement, speech problems, and mental illness. These signs and symptoms vary widely among people with late-onset forms of Sandhoff disease.
Symptoms[]
Symptoms of Sandhoff disease can appear in childhood, adolescence and in adulthood. The symptoms are motor weakness, startle reaction to sound, early blindness, progressive mental and motor deterioration, frequent respiratory infections, macrophaly (which is and enlarged head),doll-like facial appearance, seizures, cherry red spots, myoclonus (muscle contractions), enlarged liver and spleen. These symptoms are much like Tay-Sachs disease. The diseases are both inherited, and both deal with the central nervous system.
Causes[]
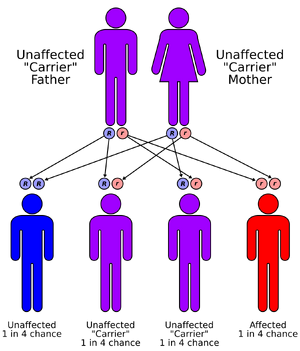
Sandhoff disease is inherited in an autosomal recessive fashion
Mutations in the HEXB gene cause Sandhoff disease. The HEXB gene provides instructions for making a protein that is part of two critical enzymes in the nervous system. These enzymes, beta-hexosaminidase A and beta-hexosaminidase B, function in nerve cells to break down fatty substances, complex sugars, and molecules that are linked to sugars. In particular, beta-hexosaminidase A breaks down a fatty compound called GM2 ganglioside. Mutations in the HEXB gene disrupt the activity of these enzymes, preventing the breakdown of GM2 ganglioside and other molecules.
As a result, these compounds can accumulate to toxic levels within cells. Progressive damage caused by the buildup of GM2 ganglioside leads to the destruction of nerve cells, which causes the signs and symptoms of Sandhoff disease. The condition is inherited in an autosomal recessive pattern.
Incidence[]
Sandhoff disease is a rare disorder; its frequency varies among populations. This condition appears to be more common in the Creole population of northern Argentina; the Metis Indians in Saskatchewan, Canada; and people from Lebanon. It is also found in Eastern Europe, Ashkenazi Jewish, but it does not limit any other ethnic groups.
Diagnosis[]
Sandhoff disease is determined by doing the following procedures before being detected by an examination, biopsy removing a sample of tissue from the liver, genetic testing, molecular analysis of cells and tissues to determine if it is a genetic metabolic disorder, enzyme assay, and sometimes an urinalysis may be done to determine if some of the materials are stored within the body. For a child to obtain this disease and both parents are carriers is only a 25 percent chance their child would inherit Sandhoff disease. The parents are given the opportunity to have a DNA mutation done if they are at high risk, so they can determine before they have children. However, it is highly recommended to get a test done even if you do not have a family history of Sandhoff disease. Over 95% of the families that have children that are facing the Sandhoff disease had no family history of it, due to the HEXB gene being a silent mutation that is passed through the genes without one knowing it has occurred. Of course, if you have the gene you have a greater risk of transmitting the gene to the unborn child. Genetic counseling is highly recommended with those who have the gene, and those who found out they have the gene after being tested.
Treatment[]
Sandhoff disease does not attain a specific treatment or cure. However, a person that is suffering from this disease needs to acquire proper nutrition, stay hydrated, and maintain clearing in the airways. To reduce some symptoms that may occur with Sandhoff disease the patient may be required to take a anticonvulsants to manage seizures, medications to treat respiratory infections in infants usually dying by the age of 3 due to respiratory infections itself, and obtain a precise diet consisting of puree foods due to difficulties swallowing.
Recent work done at Burham Institute for Medical Research and scheduled to be published in Nature, indicates that human embryonic stem cells may provide a potential therapy for the disease.
Stem cell transplants, if done at a young enough age, have been shown to arrest progression of the disease and kids can go on to have a normal lifespan. Dr. Joanne Kurtzburg at Duke University has performed these transplants on Sandhoff's children as well as Tay-Sachs children.
See also[]
- GM2-gangliosidosis, AB variant
- globoside
References[]
Madison foundation-[2] NINDS Sandhoff disease-[3] Related Diseases What is Sandhoff disease-[4] Konrad Sandhoff [5] HealthLink Medical School of Wisconsin [6]
External links[]
This article incorporates public domain text from The U.S. National Library of Medicine
amino-acids Phenylketonuria - Alkaptonuria - Ochronosis - Tyrosinemia - Maple syrup urine disease - Propionic acidemia - Methylmalonic acidemia - Isovaleric acidemia - Primary carnitine deficiency - Cystinuria - Cystinosis - Hartnup disease - Homocystinuria - Citrullinemia - Hyperammonemia - Glutaric acidemia type 1
carbohydrates Lactose intolerance - Glycogen storage disease (type I, type II, type III, type IV, type V), Fructose intolerance, Galactosemia
Lipid storage disorders Gangliosidosis - GM2 gangliosidoses (Sandhoff disease, Tay-Sachs disease) - GM1 gangliosidoses - Mucolipidosis type IV - Gaucher's disease - Niemann-Pick disease - Farber disease - Fabry's disease - Metachromatic leukodystrophy - Krabbe disease - Neuronal ceroid lipofuscinosis - Batten disease - Cerebrotendineous xanthomatosis - Wolman disease - Cholesteryl ester storage disease
List of fatty acid metabolism disorders - Hyperlipidemia - Hypercholesterolemia - Familial hypercholesterolemia - Xanthoma - Combined hyperlipidemia - Lecithin cholesterol acyltransferase deficiency - Tangier disease - Abetalipoproteinemia
mineral metabolism Disorders of calcium metabolism - Hypophosphatemia - Hypophosphatasia - Wilson's disease - Menkes disease - Hypermagnesemia - Hypomagnesemia - Hypercalcaemia - Hypocalcaemia
fluid, electrolyte and acid-base balance Electrolyte disturbance - Hypernatremia - Hyponatremia - Respiratory acidosis - Metabolic acidosis - Lactic acidosis - Hypervolemia - Hypokalemia - Hyperkalemia - Mixed disorder of acid-base balance - Hyperchloremia - Hypochloremia - Dehydration
porphyrin and bilirubin Acatalasia - Gilbert's syndrome - Crigler-Najjar syndrome - Dubin-Johnson syndrome - Rotor syndrome - Porphyria (Acute intermittent porphyria, Gunther's disease, Porphyria cutanea tarda, Erythropoietic protoporphyria, Hepatoerythropoietic porphyria, Hereditary coproporphyria, Variegate porphyria)
glycosaminoglycan Mucopolysaccharidosis - Hurler syndrome - Hunter syndrome - Sanfilippo syndrome - Morquio syndrome
glycoprotein I-cell disease - Pseudo-Hurler polydystrophy - Aspartylglucosaminuria - Fucosidosis - Alpha-mannosidosis - Sialidosis
other Alpha 1-antitrypsin deficiency - Cystic fibrosis - Familial Mediterranean fever - Lesch-Nyhan syndrome
| This page uses Creative Commons Licensed content from Wikipedia (view authors). |