Assessment |
Biopsychology |
Comparative |
Cognitive |
Developmental |
Language |
Individual differences |
Personality |
Philosophy |
Social |
Methods |
Statistics |
Clinical |
Educational |
Industrial |
Professional items |
World psychology |
Biological: Behavioural genetics · Evolutionary psychology · Neuroanatomy · Neurochemistry · Neuroendocrinology · Neuroscience · Psychoneuroimmunology · Physiological Psychology · Psychopharmacology (Index, Outline)
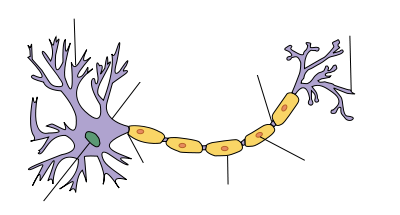
| Myelin sheath of a healthy neuron |
|---|
| Structure of a typical neuron |
Multiple sclerosis is a condition in which the CNS of a person present a special kind of distributed lesions (sclerosis) whose pathophysiology is complex and still under investigation. It is considered a pathological entity by some authors[1] and a clinical entity by some others.[2]
Damage occurs in two phases. First some MRI-abnormal areas with hidden damage appear in the brain and spine (NAWM, NAGM, DAWM), followed later by leaks in the blood–brain barrier where immune cells infiltrate causing the known demyelination.[3]
MS is mainly a white matter disease, and lesions appear mainly in a peri-ventricular distribution (lesions clustered around the ventricles of the brain), but apart of the usually known white matter demyelination, also the cortex and deep gray matter (GM) nuclei are affected, together with diffuse injury of the normal-appearing white matter.[4] MS is active even during remission periods.[5] GM atrophy is independent of the MS lesions and is associated with physical disability, fatigue, and cognitive impairment in MS[6]
At least five characteristics are present in CNS tissues of MS patients: Inflammation beyond classical white matter lesions, Intrathecal Ig production with oligoclonal bands, An environment fostering immune cell persistence, Follicle-like aggregates in the meninges and a disruption of the blood–brain barrier also outside of active lesions.[7]
Demyelination process and specific areas of damage[]
Demyelinization by MS. The Klüver-Barrera colored tissue show a clear decoloration in the area of the lesion (Original scale 1:100)
Demyelinization by MS. The CD68 colored tissue shows several Macrophages in the area of the lesion. Original scale 1:100
Damage occurs in two phases. First some MRI-abnormal areas with hidden damage appear in the brain and spine (NAWM, NAGM, DAWM), followed later by leaks in the blood–brain barrier where immune cells infiltrate causing the known demyelination.[3]
According to the view of most researchers, a special subset of lymphocytes, called T helper cells, specifically Th1 and Th17,[8] play a key role in the development of the lesion. A protein called Interleukin 12 is responsible for the differentiation of naive T cells into inflammatory T cells. An over production of this protein is what causes the increased inflammation in MS patients.[9] Under normal circumstances, these lymphocytes can distinguish between self and non-self. However, in a person with MS, these cells recognize healthy parts of the central nervous system as foreign and attack them as if they were an invading virus, triggering inflammatory processes and stimulating other immune cells and soluble factors like cytokines and antibodies. Many of the myelin-recognizing T cells belong to a terminally differentiated subset called co-stimulation-independent effector-memory T cells.[10][11][12][13][14][15][16][17][18][19][20] Recently other type of immune cells, B Cells, have been also implicated in the pathogenesis of MS[21] and in the degeneration of the axons.[22]
The axons themselves can also be damaged by the attacks.[23] Often, the brain is able to compensate for some of this damage, due to an ability called neuroplasticity. MS symptoms develop as the cumulative result of multiple lesions in the brain and spinal cord. This is why symptoms can vary greatly between different individuals, depending on where their lesions occur.
Repair processes, called remyelination, also play an important role in MS. Remyelination is one of the reasons why, especially in early phases of the disease, symptoms tend to decrease or disappear temporarily. Nevertheless, nerve damage and irreversible loss of neurons occur early in MS.
The oligodendrocytes that originally formed a myelin sheath cannot completely rebuild a destroyed myelin sheath. However, the central nervous system can recruit oligodendrocyte stem cells capable of proliferation and migration and differentiation into mature myelinating oligodendrocytes. The newly-formed myelin sheaths are thinner and often not as effective as the original ones. Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons. Under laboratory conditions, stem cells are quite capable of proliferating and differentiating into remyelinating oligodendrocytes; it is therefore suspected that inflammatory conditions or axonal damage somehow inhibit stem cell proliferation and differentiation in affected areas[24]
Brain lesions distribution[]
Dawson's Fingers appearing on an MRI scan
Multiple sclerosis is considered a disease of the white matter because normally lesions appear in this area, but it is also possible to find some of them in the grey matter.[25]
Using high field MRI system, with several variants several areas show lesions, and can be spacially classified in infratentorial, callosal, juxtacortical, periventricular, and other white matter areas.[26] Other authors simplify this in three regions: intracortical, mixed gray-white matter, and juxtacortical.[27] Others classify them as hippocampal, cortical, and WM lesions,[28] and finally, others give seven areas: intracortical, mixed white matter-gray matter, juxtacortical, deep gray matter, periventricular white matter, deep white matter, and infratentorial lesions.[29] The distribution of the lesions could be linked to the clinical evolution[30]
Post-mortem autopsy reveal that gray matter demyelination occurs in the motor cortex, cingulate gyrus, cerebellum, thalamus and spinal cord.[31] Cortical lesions have been observed specially in people with SPMS but they also appear in RRMS and clinically isolated syndrome. They are more frequent in men than in women[32] and they can partly explain cognitive deficits.
It is known that two parameters of the cortical lesions, fractional anisotropy (FA) and mean diffusivity (MD), are higher in patients than in controls.[33] They are larger in SPMS than in RRMS and most of them remain unchanged for short follow-up periods. They do not spread into the subcortical white matter and never show gadolinium enhancement. Over a one-year period, CLs can increase their number and size in a relevant proportion of MS patients, without spreading into the subcortical white matter or showing inflammatory features similar to those of white matter lesions.[34]
Due to the distribution of the lesions, since 1916 they are also known as Dawson's fingers.[35] They appear around the brain blood vessels.
Spinal cord damage[]
Cervical spinal cord has been found to be affected by MS even without attacks, and damage correlates with disability.[36] In RRMS, cervical spinal cord activity is enhanced, to compensate for the damage of other tissues.[37] It has been shown that Fractional anisotropy of cervical spinal cord is lower than normal, showing that there is damage hidden from normal MRI.[38]
Progressive tissue loss and injury occur in the cervical cord of MS patients. These two components of cord damage are not interrelated, suggesting that a multiparametric MRI approach is needed to get estimates of such a damage. MS cord pathology is independent of brain changes, develops at different rates according to disease phenotype, and is associated to medium-term disability accrual.[39]
Spinal cord presents grey matter lesions, that can be confirmed post-mortem and by high field MR imaging. Spinal cord grey matter lesions may be detected on MRI more readily than GM lesions in the brain, making the cord a promising site to study the grey matter demyelination.[40]
Retina and optic nerve damage[]
There is axonal loss in the retina and optic nerve, which can be meassured by Optical coherence tomography[41] or by Scanning laser polarimetry.[42] This measure can be used to predict disease activity[43] and to establish a differential diagnosis from Neuromyelitis optica[44]
In vertebrate embryonic development, the retina and the optic nerve originate as outgrowths of the developing brain, so the retina is considered part of the central nervous system (CNS).[45] It is the only part of the CNS that can be imaged non-invasively in the living organism.
The retina is unique within the CNS in that it contains axons and glia but no myelin, and it is, therefore, an ideal structure within which to visualize the processes of neurodegeneration.[46] Tissue-bound IgG was demonstrated on retinal ganglion cells in six of seven multiple sclerosis cases but not in controls.[47]
Uveitis and retinal phlebitis are manifestations of MS. Trypsin digestion with microscopic examination is a method of testing for phlebitis and the frequency found in this series is higher than in others. These lesions are similar to the perivenular cuffing that occurs in the central nervous system in MS.[48]
Retinal vessels show narrower arterioles and wider venules even in absence of optic neuritis, possibly as a consequence of subclinical swelling of optic nerve axons,[49] together with a higher than normal rigidity[50]
Neural and axonal damage[]
The axons of the neurons are damaged probably by B-Cells,[22] though currently no relationship has been established with the relapses or the attacks.[23] It seems that this damage is a primary target of the immune system, i.e. not secondary damage after attacks against myelin,[51] though this has been disputed[52]
Proton magnetic resonance spectroscopy has shown that there is widespread neuronal loss even at the onset of MS, largely unrelated to inflammation.[53]
A relationship between neural damage and N-Acetyl-Aspartate concentration has been established, and this could lead to new methods for early MS diagnostic through magnetic resonance spectroscopy[54]
Axonal degeneration at CNS can be estimated by N-acetylaspartate to creatine (NAA/Cr) ratio, both measured by with proton magnetic resonance spectroscopy.[55]
Peripheral nervous system involvement[]
Though MS is defined as a CNS condition, some reports link problems in the peripheral nervous system with the presence of MS plaques in the CNS[56]
Lesion structure[]
Layers of a lesion
Multiple sclerosis is a condition defined by the presence of a special kind of lesions in the brain and spinal cord.[2] Therefore it is very important to establish what those "lesions typical of MS" are. They mainly consist in demyelination and scarring in the fatty myelin sheaths around the axons of the brain and spinal cord.[57] According with the most recent research, an active lesion is composed of different layers[58]:
- NAWM border with the lesion: These areas contained activated microglia, antibodies binding to astrocytes, axons, oligodendrocytes and dendritic cells along blood vessels. No T or B cells are present.
- Lesion external layer: Number of oligodendrocyte cell bodies decreases. Remaining oligodendrocytes are sometimes swollen or dying. Myelin sheaths are still intact but swollen. Small increase in microglia and T cells.
- Active layer: Phagocytic demyelinating areas: There is myelin debris taken up by local microglia and phagocytes entering from the bloodstream. More T cells in these areas, and in the space adjacent to blood vessels.
- Recently demyelinated tissue: Tissues were full of myelin-containing phagocytes. Signs of early remyelination together with small numbers of oligodendrocytes. Large numbers of T cells, B cells, and other immune cells concentrated around blood vessels.
- Inactive layer: Again activated microglia and dendritic cells were also found around blood vessels.
Lesions under MRI[]
Most MS lesions are isointense to white matter (they appear bright) on T1-weighted MRI, but some are "hypointense" (lower intensity). These are called "black holes" (BH). They appear specially in the supratentorial region of the brain.
When BH's appear, around half of them revert in a month. This is considered a sign of remyelination. When they remain, this is regarded as a sign of permanent demyelination and axonal loss. This has been shown on post-mortem autopsies.[59]
Small lesions are invisible under MRI. Therefore clinically assisted diagnostic criteria are still required for a more accurate MS diagnosis than MRI alone.[60]
Blood–brain barrier disruption[]
A healthy blood–brain barrier (BBB) should not allow T-cells to enter the nervous system. BBB disruption is the moment in which T-cells cross the barrier and has always been considered one of the early problems in the MS lesions. For unknown reasons, leaks appear in the BBB during the course of MS.[61]
Recently it has been found that BBB damage happens even in non-enhancing lesions.[62] MS has an important vascular component.[63]
The BBB is built up of endothelial cells lining the blood vessel walls. After its breakdown several problems appear, such as swelling, activation of macrophages, and more activation of cytokines and other proteins such as matrix metalloproteinases which are destructive.[64]
Whatever the demyelination process is, currently it is possible to detect lesions before demyelination, and they show clusters of activated microglia and leukocyte infiltration, together with oligodendrocytes abnormalities[65]
As lesions appear (using MRI) in "Normal-appearing white matter" (NAWM), there is supposed to be the cause that finally triggers the BBB disruption.[66] The damaged white matter is known as "Normal-appearing white matter" (NAWM) and is where lesions appear.[3] These lesions form in NAWM before blood–brain barrier breakdown.[67]
BBB can be broken centripetally or centrifugally, the first form being the most normal.[68] Several possible biochemical disrupters have been proposed. Some hypothesis about how the BBB is compromised revolve around the presence of different compounds in the blood that could interact with the vascular vessels ony in the NAWM areas. The permeability of two cytokines, Interleukin 15 and LPS, could be involved in the BBB breakdown.[69] The BBB breakdown is responsible for monocyte infiltration and inflammation in the brain.[70] Monocyte migration and LFA-1-mediated attachment to brain microvascular endothelia is regulated by SDF-1alpha through Lyn kinase[71]
Using iron nanoparticles, involvement of macrophages in the BBB breakdown can be detected.[72] A special role is played by Matrix metalloproteinases. These are a group of proteases that increase T-cells permeability of the blood–brain barrier, specially in the case of MMP-9,[64] and are supposed to be related to the mechanism of action of interferons.[73]
Whether BBB dysfunction is the cause or the consequence of MS[74] is still disputed,because activated T-Cells can cross a healthy BBB when they express adhesion proteins.[75] Apart from that, activated T-Cells can cross a healthy BBB when they express adhesion proteins.[75] (Adhesion molecules could also play a role in inflammation[76]) In particular, one of these adhesion proteins involved is ALCAM (Activated Leukocyte Cell Adhesion Molecule, also called CD166), and is under study as therapeutic target.[77] Other protein also involved is CXCL12,[78] which is found also in brain biopsies of inflammatory elements,[79] and which could be related to the behavior of CXCL13 under methylprednisolone therapy.[80] Some molecular biochemical models for relapses have been proposed.[81]
Normally, gadolinium enhancement is used to show BBB disruption on MRIs.[82] Abnormal tight junctions are present in both SPMS and PPMS. They appear in active white matter lesions, and gray matter in SPMS. They persist in inactive lesions, particularly in PPMS.[83]
A deficiency of uric acid has been implicated in this process. Uric acid added in physiological concentrations (i.e. achieving normal concentrations) is therapeutic in MS by preventing the breakdown of the blood brain barrier through inactivation of peroxynitrite.[84] The low level of uric acid found in MS victims is manifestedly causative rather than a consequence of tissue damage in the white matter lesions,[85] but not in the grey matter lesions.[86] Besides, uric acid levels are lower during relapses.[87]
Damage before BBB disruption[]
Special MRI methods[]
Before BBB disruption, brain tissues present normal aspect under normal MRI (Normal appearing white matter, NAWM and normal appearing grey matter, NAGM), but show several abnormalities under special MRI technologies:
Magnetization transfer multi-echo T(2) relaxation. Subjects with Long-T(2) lesions had a significantly longer disease duration than subjects without this lesion subtype.[88] It has been found that grey matter injury correlates with disability[89] and that there is high oxidative stress in lesions, even in the old ones.[90]
Diffusion tensor MRI or Magnetic Transfer MRI are two options to enhance MRI-hidden abnormalities discovery. This is currently an active field of research with no definitive results, but it seems that these two technologies are complementary.[91]
Other methods of MRI allow us to get a better insight of the lesions structure. Recently MP-RAGE MRI has shown better results than PSIR and DIR for gray matter lesions.[92] Susceptibility weighted imaging (SWI-MRI) has shown iron (hemosiderin) deposition in lesions, and helps to detect otherwise invisible lesions.[93]
Normal appearing brain tissues[]
Using several texture analysis technologies, it is possible to classify white matter areas into three categories: normal, normal-appearing and lesions.[94] Currently, it is possible to detect lesions before they present demyelination, and they are called pre-active lesions.[65] A fourth area called DAWM (diffusely abnormal white matter) has recently been proposed[95] and can help to differentiate PPMS and SPMS.[96] Abundant extracellular myelin in the meninges of patients with multiple sclerosis has been found[97]
Brain tissues with MRI-hidden problems are usually named Normal Appearing. Exploring the normal-appearing corpus callosum has been found a possible primary hypoperfusion,[98][99] according with other findings in this same direction.[100][101][102][103][104][105] Also iron (in hemosiderin deposits and as well as in ferritin-like structures inside the macrophage) accumulation has been reported[106][107]
Several findings in these areas have been shown. Post-mortem studies over NAWM and NAGM areas (Normal appearing White and Gray Matters) show several biochemical alterations, like increased protein carbonylation and high levels of Glial fibrillary acidic protein (GFAP), which in NAGM areas comes together with higher than normal concentration of protein carbonyls, suggesting reduced levels of antioxidants and the presence of small lesions.[108] The amount of interneuronal Parvalbumin is lower than normal in brain's motor cortex areas,[109] and oxidative injury of oligodendrocytes and neurons could be associated with active demyelination and axonal injury.[110]
Normal appearing White Matter[]
The white matter with hidden but MRI-visible damage is known as "Normal-appearing white matter" (NAWM) and is where lesions appear.[3]
BBB disruption takes place on NAWM areas.[66] This can be read in different ways. Maybe some hidden changes in White Matter structure trigger the BBB disruption, or maybe the same process that creates the NAWM areas disrupts the BBB after some time.
Pre-active lesions are lesions in an early stage of development. They resolve sometimes without further damage, and not always develop into demyelinating lesions.[65] They present clusters of activated microglia in otherwise normal-appearing white matter.
Oligodendrocyte abnormalities appear to be crucially involved.[67][111] The earliest change reported in the lesions examined is widespread oligodendrocyte apoptosis in which T cells, macrophages, activated microglia, reactive astrocytes, and neurons appear normal. This observation points to some change in the local environment (NAWM) to which oligodendrocytes are especially susceptible and which triggers a form of apoptosis.[112]
Water diffusivity is higher in all NAWM regions, deep gray matter regions, and some cortical gray matter region of MS patients than normal controls.[113]
Citrullination appears in SPMS.[114] It seems that a defect of sphingolipid metabolism modifies the properties of normal appearing white matter.[115] Related to these, peptidylarginine deiminase 2 is increased in patients with MS, and is related to arginine de-imination.[116]
NAWM shows a decreased perfusion which does not appear to be secondary to axonal loss.[103] The reduced perfusion of the NAWM in MS might be caused by a widespread astrocyte dysfunction, possibly related to a deficiency in astrocytic beta(2)-adrenergic receptors and a reduced formation of cAMP, resulting in a reduced uptake of K(+) at the nodes of Ranvier and a reduced release of K(+) in the perivascular spaces.[117] This would be consistent again with cases of Chronic cerebrospinal venous insufficiency.
White matter lesions appear in NAWM areas,[3] and their behavior can be predicted by MRI parameters as MTR (magnetization transfer ratio).[118][119] This MTR parameter is related to axonal density.[120]
It also seems that myelin basic protein (MBP) from multiple sclerosis (MS) patients contains lower levels of phosphorylation at Thr97 than normal individuals.[121]
Gray matter damage. Normal Appearing Gray Matter[]
Gray matter tissue damage dominates the pathological process as MS progresses, and underlies neurological disability. Imaging correlates of gray matter atrophy indicate that mechanisms differ in RRMS and SPMS.[122] Epstein-Barr virus could be involved,[123] but is not likely.[124] Involvement of the deep gray matter (DGM), suggested by magnetic resonance imaging, is confirmed, and most DGM lesions involve both GM and white matter. Inflammation in DGM lesions is intermediate between the destructive inflammation of white matter lesions and the minimal inflammation of cortical lesions.[125]
Iron depositions appear in deep gray matter by magnetic field correlation MRI[126]
Diffusely abnormal white matter[]
Other active area of study is the Diffusely abnormal white matter (DAWM). It seems to be a reduction of myelin phospholipids that correlates with a reduction of the myelin water fraction.[127] The DAWM consisted of extensive axonal loss, decreased myelin density, and chronic fibrillary gliosis, all of which were substantially abnormal compared with normal-appearing WM and significantly different from focal WM lesion pathology.[128] Changes in the vasculature take place not only in focal lesions but also in DAWM as detected by postmortem MRI[129]
Origin of the normal-appearing tissues[]
The cause why the normal appearing areas appear in the brain is unknown. Historically, several theories about how this happens has been presented.
Old blood flow theories[]
Venous pathology has been associated with MS for more than a century. Pathologist Georg Eduard Rindfleisch noted in 1863 that the inflammation-associated lesions were distributed around veins.[130] Some other authors like Tracy Putnam[131] pointed to venous obstructions.
Some authors like Franz Schelling proposed a mechanical damage procedure based on violent blood reflux.[132] Later the focus moved to softer hemodynamic abnormalities, which were shown that precede changes in sub-cortical gray matter[102] and in substantia nigra.[133] However, such reports of a "hemodynamic cause of MS" are not universal, and possibly not even common. At this time the evidence is largely anecdotal and some MS patients have no blood flow issues. Possibly vascular problems may be an aggravating factor, like many others in MS. Indeed the research, by demonstrating patients with no hemodynamic problems actually prove that this is not the only cause of MS.
Endothelium theories[]
Other theories point to a possible primary endothelial disfunction.[134] The importance of vascular misbehaviour in MS pathogenesis has also been independently confirmed by seven-tesla MRI.[135] It is reported that a number of studies have provided evidence of vascular occlusion in MS, which suggest the possibility of a primary vascular injury in MS lesions or at least that they are occasionally correlated.[136]
Some morphologically special medullar lesions (wedge-shaped) have also been linked to venous insufficiency.[137]
CCSVI[]
The term "chronic cerebrospinal venous insufficiency" was coined in 2008 by Paolo Zamboni, who described it in patients with multiple sclerosis. Instead of intracranial venous problems he described extracranial blockages, and he stated that the location of those obstructions seemed to influence the clinical course of the disease.[138] According to Zamboni, CCSVI had a high sensitivity and specificity differentiating healthy individuals from those with multiple sclerosis.[139] Zamboni's results were criticized as some of his studies were not blinded and they need to be verified by further studies.[138][139] As of 2010[update]Template:Dated maintenance category the theory is considered at least defensible[140]
A more detailed evidence of a correlation between the place and type of venous malformations imaged and the reported symptoms of multiple sclerosis in the same patients was published in 2010.[141]
Haemodynamic problems have been found in the blood flow of MS patients using Doppler,[142] initially using transcranial color-coded duplex sonography (TCCS), pointing to a relationship with a vascular disease called chronic cerebro-spinal venous insufficiency (CCSVI).[143][144] In 2010 there were conflicting results when evaluating the relationship between MS and CCSVI.[145][146][147][148] but is important to note that positives have appeared among the blinded studies.
CSF flow theories[]
Other theories focus in the possible role of cerebrospinal fluid flow impairment.[149] This theory could be partially consistent with the previous one[150]
Currently a small trial with 8 participants has been performed[151]
Molecular biomarkers[]
Diagnosis of MS has always been made by clinical examination, supported by MRI or CSF tests. According with the autoimmune hypothesis, researchers expect to find biomarkers able to yield a better diagnosis. As of 2009 no biomarker with perfect correlation has been found, but some of them have shown a special behavior.
In blood[]
Blood serum of MS patients shows abnormalities. Endothelin-1 shows maybe the most striking discordance between patients and controls, being a 224% higher in patients than controls.[152]
Creatine and Uric acid levels are lower than normal, at least in women.[153] Ex vivo CD4(+) T cells isolated from the circulation show a wrong TIM-3 (Immunoregulation) behavior,[154] and relapses are associated with CD8(+) T Cells.[155] There is a set of differentially expressed genes between MS and healthy subjects in peripheral blood T cells from clinically active MS patients. There are also differences between acute relapses and complete remissions.[156] Platelets are known to have abnormal high levels.[157]
MS patients are also known to be CD46 defective, and this leads to Interleukin-10 (IL-10) deficiency, being this involved in the inflammatory reactions.[158] Levels of IL-2, IL-10, and GM-CSF are lower in MS females than normal. IL6 is higher instead. These findings do not apply to men.[159] This IL-10 interleukin could be related to the mechanism of action of methylprednisolone, together with CCL2. Interleukin IL-12 is also known to be associated with relapses, but this is unlikely to be related to the response to steroids[160]
Kallikreins are found in serum and are associated with secondary progressive stage.[161] Related to this, it has been found that B1-receptors, part of the kallikrein-kinin-system, are involved in the BBB breakdown[162][163]
There is evidence of Apoptosis-related molecules in blood and they are related to disease activity.[164] B cells in CSF appear, and they correlate with early brain inflammation.[165] There is also an overexpression of IgG-free kappa light chain protein in both CIS and RR-MS patients, compared with control subjects, together with an increased expression of an isoforms of apolipoprotein E in RR-MS.[166] Expression of some specific proteins in circulating CD4+ T cells is a risk factor for conversion from CIS to clinically defined multiple sclerosis.[167]
Recently, unique autoantibody patterns that distinguish RRMS, secondary progressive (SPMS), and primary progressive (PPMS) have been found, based on up- and down-regulation of CNS antigens,[168] tested by microarrays. In particular, RRMS is characterized by autoantibodies to heat shock proteins that were not observed in PPMS or SPMS. These antibodies patterns can be used to monitor disease progression.[169][170]
Finally, a promising biomarker under study is an antibody against the potassium channel protein KIR4.1[171]. This biomarker has been reported to be present in around a half of MS patients, but in nearly none of the controls.
In blood vessels tissue[]
Endothelial disfunction has been reported in MS[172] and could be used as biomarker via biopsia. Blood circulation is slower in MS patients and can be meassured using contrast[173] or by MRI[174]
In Cerebrospinal Fluid[]
It has been known for quite some time that glutamate is present at higher levels in CSF during relapses[175] compared to healthy subjects and to MS patients before relapses. Also a specific MS protein has been found in CSF, chromogranin A, possibly related to axonal degeneration. It appears together with clusterin and complement C3, markers of complement-mediated inflammatory reactions.[176] Also Fibroblast growth factor-2 appear higher at CSF.[177]
CSF also shows oligoclonal bands (OCB) in the majority (around 95%) of the patients. Several studies have reported differences between patients with and without OCB with regard to clinical parameters such as age, gender, disease duration, clinical severity and several MRI characteristics, together with a varying lesion load.[178]
Varicella-zoster virus particles have been found in CSF of patients during relapses, but this particles are virtually absent during remissions.[179] Plasma Cells in the cerebrospinal fluid of MS patients could also be used for diagnosis, because they have been found to produce myelin-specific antibodies.[180] As of 2011, a recently discovered myelin protein TPPP/p25, has been found in CSF of MS patients[181]
In brain cells[]
Abnormal sodium distribution has been reported in living MS brains. In the early-stage RRMS patients, sodium MRI revealed abnormally high concentrations of sodium in brainstem, cerebellum and temporal pole. In the advanced-stage RRMS patients, abnormally high sodium accumulation was widespread throughout the whole brain, including normal appearing brain tissue[182]. It is currently unknown wether post-mortem brains are consistent with this observation.
Subgroups by molecular biomarkers[]
Differences have been found between the proteines expressed by patients and healthy subjects, and between attacks and remissions. Using DNA microarray technology groups of molecular biomarkers can be established.[183] For example, it is known that Anti-lipid oligoclonal IgM bands (OCMB) distinguish MS patients with early aggressive course and that these patients show a favourable response to immunomodulatory treatment.[184]
It seems that Fas and MIF are candidate biomarkers of progressive neurodegeneration. Upregulated levels of sFas (soluble form of Fas molecule) were found in MS patients with hypotense lesions with progressive neurodegeneration, and also levels of MIF appeared to be higher in progressive than in non-progressing patients. Serum TNF-α and CCL2 seem to reflect the presence of inflammatory responses in primary progressive MS.[185]
Heterogeneity of the disease[]
Multiple sclerosis has been reported to be heterogeneus in its behavior, in its underlying mechanisms and recently also in its response to medication.[186]
Four different damage patterns have been identified by her team in the scars of the brain tissue. Understanding lesion patterns can provide information about differences in disease between individuals and enable doctors to make more accurate treatment decisions. According to one of the researchers involved in the original research "Two patterns (I and II) showed close similarities to T-cell-mediated or T-cell plus antibody-mediated autoimmune encephalomyelitis, respectively. The other patterns (III and IV) were highly suggestive of a primary oligodendrocyte dystrophy, reminiscent of virus- or toxin-induced demyelination rather than autoimmunity."
Also known as Lassmann patterns,[187] it is believed that they may correlate with differences in disease type and prognosis, and perhaps with different responses to treatment. This report suggests that there may be several types of MS with different immune-related causes, and that MS may be a family of several diseases. The four identified patterns are [19]:
- Pattern I
- The scar presents T-cells and macrophages around blood vessels, with preservation of oligodendrocytes, but no signs of complement system activation.[188]
- Pattern II
- The scar presents T-cells and macrophages around blood vessels, with preservation of oligodendrocytes, as before, but also signs of complement system activation can be found.[189] Though this pattern could be considered similar to damage seen in NMO, some authors report no AQP4 damage in pattern II lesions[190]
- Pattern III
- The scars are diffuse with inflammation, distal oligodendrogliopathy and microglial activation. There is also loss of myelin-associated glycoprotein (MAG). The scars do not surround the blood vessels, and in fact, a rim of preserved myelin appears around the vessels. There is evidence of partial remyelinization and oligodendrocyte apoptosis. For some researchers this pattern is an early stage of the evolution of the others.[112]
- Pattern IV
- The scar presents sharp borders and oligodendrocyte degeneration, with a rim of normal appearing white matter. There is a lack of oligodendrocytes in the center of the scar. There is no complement activation or MAG loss.
The meaning of this fact is controversial. For some investigation teams it means that MS is a heterogeneous disease. Others maintain that the shape of the scars can change with time from one type to other and this could be a marker of the disease evolution.[191] Anyway, the heterogeneity could be true only for the early stage of the disease.[192] Some lesions present mitocondrial defects that could distinguish types of lesions.[193] Currently antibodies to lipids and peptides in sera, detected by microarrays, can be used as markers of the pathological subtype given by brain biopsy.[169]
Several correlations have been studied:
- With clinical courses: No definitive relationship between these patterns and the clinical subtypes has been established by now, but some relations have been established. All the cases with PPMS (primary progressive) had pattern IV (oligodendrocyte degeneration) in the original study[194] and nobody with RRMS was found with this pattern. Balo concentric sclerosis lesions have been classified as pattern III (distal oligodendrogliopathy).[195] Neuromyelitis optica was associated with pattern II (complement mediated demyelination), though they show a perivascular distribution, at difference from MS pattern II lesions.[196]
- With MRI and MRS findings: The researchers are attempting this with magnetic resonance images to confirm their initial findings of different patterns of immune pathology and any evidence of possible disease "sub-types" of underlying pathologies. It is possible that such "sub-types" of MS may evolve differently over time and may respond differently to the same therapies. Ultimately investigators could identify which individuals would do best with which treatments. It seems that Pulsed magnetization transfer imaging,[197] diffusion Tensor MRI,[198] and VCAM-1 enhanced MRI[199] could be able to show the pathological differences of these patterns. Together with MRI, magnetic resonance spectroscopy will allow in the future to see the biochemical composition of the lesions.
- With CSF findings: Teams in Oxford and Germany,[200] found correlation with CSF and progression in November 2001, and hypotheses have been made suggesting correlation between CSF findings and pathophysiological patterns.[201] In particular, B-cell to monocyte ratio looks promising. The anti-MOG antibody has been investigated but no utility as biomarker has been found,[202] though this is disputed.[203] High levels of anti-nuclear antibodies are found normally in patients with MS[citation needed]. Antibodies against Neurofascin–186 could be involved in a subtype of MS[204]
- With responses to therapy: It is known that 30% of MS patients are non-responsive to Beta interferon.[205] The heterogeneous response to therapy can support the idea of hetherogeneous aetiology. It has also been shown that IFN receptors and interleukins in blood serum predicts response to IFN therapy,[206][207], specially IL-17[208], and interleukins IL12/IL10 ratio has been proposed as marker of clinical course.[209] Besides:
- Pattern II lesions patients are responsive to plasmapheresis, while others are not.[210][211]
- The subtype associated with macrophage activation, T cell infiltration and expression of inflammatory mediator molecules may be most likely responsive to immunomodulation with interferon-beta or glatiramer acetate.[212]
- People non-responsive to interferons are the most responsive to Copaxone [20][213]
- In general, people non-responsive to a treatment is more responsive to other,[214] and changing therapy can be effective.[215]
- There are genetic differences between responders and not responders.[216] Though the article points to heterogeneous metabolic reactions to interferons instead of disease heterogeneity, it has been shown that most genetic differences are not related to interferon behavior[217]
Pathology of early MS and silent MS[]
Current McDonald criteria usually do not allow to stablish a diagnosis for definite MS before two clinical attacks have appeared. This means that for clinical definite cases, MS condition has been present for a long time, difficulting the study of the initial stages.[218] Therefore for studying this initial stage no clinical CDMS cases and pathological definitions are normally used.[1] Sometimes patients with their first isolated attack (Clinically Isolated syndrome, or CIS) are used instead.
Cases of MS before the CIS are sometimes found during other neurological inspections and are referred to as subclinical MS.,[219] or sometimes Clinically silent MS.[220] The previous reference states that clinically silent MS plaques were located in the periventricular areas. This reference also reports an estimate of the prevalence of silent MS as high as about 25%. Oligodendrocytes evolution is similar to normal MS clinical courses[221]
Also cases after the CIS but before the confirming second attack (Preclinical MS) can be accepted to study the initial MS pathology[222]
These studies are performed for ethiological research purposes and not for improving diagnosis.
See also[]
- Multiple sclerosis borderline
References[]
- ↑ 1.0 1.1 Lassmann H (2010). Acute disseminated encephalomyelitis and multiple sclerosis. Brain 133 (2): 317.
- ↑ 2.0 2.1 McDonald WI, Compston A, Edan G, et al. (2001). Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann. Neurol. 50 (1): 121–7.
- ↑ 3.0 3.1 3.2 3.3 3.4 Goodkin DE, Rooney WD, Sloan R, et al. (December 1998). A serial study of new MS lesions and the white matter from which they arise. Neurology 51 (6): 1689–97.
- ↑ Lassmann H, Brück W, Lucchinetti CF (April 2007). The immunopathology of multiple sclerosis: an overview. Brain Pathol. 17 (2): 210–8.
- ↑ Kirov I, Patil V, Babb J, Rusinek H, Herbert J, Gonen O (June 2009). MR Spectroscopy Indicates Diffuse Multiple Sclerosis Activity During Remission. J. Neurol. Neurosurg. Psychiatr. 80 (12): 1330–6.
- ↑ Pirko I, Lucchinetti CF, Sriram S, Bakshi R (February 2007). Gray matter involvement in multiple sclerosis. Neurology 68 (9): 634–42.
- ↑ Meinl E, Krumbholz M, Derfuss T, Dewitt D, (November 2008). Compartmentalization of inflammation in the CNS: A major mechanism driving progressive multiple sclerosis. J Neurol Sci. 274 (1–2): 42–4.
- ↑ Fransson ME, Liljenfeldt LS, Fagius J, Tötterman TH, Loskog AS. (2009). The T-cell pool is anergized in patients with multiple sclerosis in remission. Immunology 126 (1): 92–101.
- ↑ http://wwwchem.csustan.edu/chem4400/sjbr/corey02.htm
- ↑ Markovic-Plese S, Cortese I, Wandinger KP, McFarland HF, Martin R (October 2001). CD4+CD28– costimulation-independent T cells in multiple sclerosis. J. Clin. Invest. 108 (8): 1185–94.
- ↑ Wulff H, Calabresi PA, Allie R, et al. (June 2003). The voltage-gated Kv1.3 K+ channel in effector memory T cells as new target for MS. J. Clin. Invest. 111 (11): 1703–13.
- ↑ Rus H, Pardo CA, Hu L, et al. (August 2005). The voltage-gated potassium channel Kv1.3 is highly expressed on inflammatory infiltrates in multiple sclerosis brain. Proc. Natl. Acad. Sci. U.S.A. 102 (31): 11094–9.
- ↑ Beeton C, Chandy KG (December 2005). Potassium channels, memory T cells, and multiple sclerosis. Neuroscientist 11 (6): 550–62.
- ↑ Okuda Y, Okuda M, Apatoff BR, Posnett DN (August 2005). The activation of memory CD4(+) T cells and CD8(+) T cells in patients with multiple sclerosis. J. Neurol. Sci. 235 (1–2): 11–7.
- ↑ Krakauer M, Sorensen PS, Sellebjerg F (December 2006). CD4(+) memory T cells with high CD26 surface expression are enriched for Th1 markers and correlate with clinical severity of multiple sclerosis. J. Neuroimmunol. 181 (1–2): 157–64.
- ↑ Ratts RB, Karandikar NJ, Hussain RZ, et al. (September 2006). Phenotypic characterization of autoreactive T cells in multiple sclerosis. J. Neuroimmunol. 178 (1–2): 100–10.
- ↑ Haegele KF, Stueckle CA, Malin JP, Sindern E (February 2007). Increase of CD8+ T-effector memory cells in peripheral blood of patients with relapsing-remitting multiple sclerosis compared to healthy controls. J. Neuroimmunol. 183 (1–2): 168–74.
- ↑ Jilek S, Schluep M, Rossetti AO, et al. (April 2007). CSF enrichment of highly differentiated CD8+ T cells in early multiple sclerosis. Clin. Immunol. 123 (1): 105–13.
- ↑ {{cite journal |author=Miyazaki Y, Iwabuchi K, Kikuchi S, et al. |title=Expansion of CD4+CD28- T cells producing high levels of interferon-{gamma} in peripheral blood of patients with multiple sclerosis |journal=Mult. Scler. |volume=14 |issue=8 |pages=1044–55 |year=2008 |month=September |pmid=18573819 |doi=10.1177/1352458508092809 |url=http://msj.sagepub.com/cgi/pmidlookup?view=long&pmid=18573819}}
- ↑ Lünemann JD, Jelcić I, Roberts S, et al. (August 2008). EBNA1-specific T cells from patients with multiple sclerosis cross react with myelin antigens and co-produce IFN-γ and IL-2. J. Exp. Med. 205 (8): 1763–73.
- ↑ Hauser SL, Waubant E, Arnold DL, et al. (February 2008). B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med. 358 (7): 676–88.
- ↑ 22.0 22.1 Cause of nerve fiber damage in multiple sclerosis identified
- ↑ 23.0 23.1 Pascual AM, Martínez-Bisbal MC, Boscá I, et al. (2007). Axonal loss is progressive and partly dissociated from lesion load in early multiple sclerosis. Neurology 69 (1): 63–7.
- ↑ Wolswijk G (15 January 1998). Chronic stage multiple sclerosis lesions contain a relatively quiescent population of oligodendrocyte precursor cells. J Neurosci. 18 (2): 601–9.
- ↑ Jeroen J. G. Geurtsa, Lars Böc, Petra J. W. Pouwelsd, Jonas A. Castelijnsa, Chris H. Polmanb and Frederik Barkhof, Cortical Lesions in Multiple Sclerosis: Combined Postmortem MR Imaging and Histopathology, American Journal of Neuroradiology 26:572-577, March 2005 [1]
- ↑ Wattjes MP, Harzheim M, Kuhl CK, et al. (1 September 2006). Does high-field MR imaging have an influence on the classification of patients with clinically isolated syndromes according to current diagnostic mr imaging criteria for multiple sclerosis?. AJNR Am J Neuroradiol. 27 (8): 1794–8.
- ↑ Nelson F, Poonawalla AH, Hou P, Huang F, Wolinsky JS, Narayana PA (October 2007). Improved identification of intracortical lesions in multiple sclerosis with phase-sensitive inversion recovery in combination with fast double inversion recovery MR imaging. AJNR Am J Neuroradiol. 28 (9): 1645–9.
- ↑ Roosendaal SD, Moraal B, Vrenken H, et al. (April 2008). In vivo MR imaging of hippocampal lesions in multiple sclerosis. J Magn Reson Imaging. 27 (4): 726–31.
- ↑ Geurts JJ, Pouwels PJ, Uitdehaag BM, Polman CH, Barkhof F, Castelijns JA (July 2005). Intracortical lesions in multiple sclerosis: improved detection with 3D double inversion-recovery MR imaging. Radiology 236 (1): 254–60.
- ↑ Sampat MP, Berger AM, Healy BC, et al. (October 2009). Regional White Matter Atrophy–Based Classification of Multiple Sclerosis in Cross-Sectional and Longitudinal Data. AJNR Am J Neuroradiol 30 (9): 1731–9.
- ↑ Gilmore CP, Donaldson I, Bö L, Owens T, Lowe JS, Evangelou N (October 2008). Regional variations in the extent and pattern of grey matter demyelination in Multiple Sclerosis: a comparison between the cerebral cortex, cerebellar cortex, deep grey matter nuclei and the spinal cord. J Neurol Neurosurg Psychiatry. 80 (2): 182–7.
- ↑ Calabrese M, De Stefano N, Atzori M, et al. (2007). Detection of cortical inflammatory lesions by double inversion recovery magnetic resonance imaging in patients with multiple sclerosis. Arch. Neurol. 64 (10): 1416–22.
- ↑ Poonawalla AH, Hasan KM, Gupta RK, et al. (2008). Diffusion-Tensor MR Imaging of Cortical Lesions in Multiple Sclerosis: Initial Findings. Radiology 246 (3): 880–6.
- ↑ Calabrese M, Filippi M, Rovaris M, Mattisi I, Bernardi V, Atzori M, Favaretto A, Barachino L, Rinaldi L, Romualdi C, Perini P, Gallo P. (2008). Morphology and evolution of cortical lesions in multiple sclerosis. A longitudinal MRI study. NeuroImage 42 (4): 1324–8.
- ↑ Dawson fingers, at Radiopedia
- ↑ Agosta F, Pagani E, Caputo D, Filippi M (2007). Associations between cervical cord gray matter damage and disability in patients with multiple sclerosis. Arch. Neurol. 64 (9): 1302–5.
- ↑ Agosta F, Valsasina P, Rocca MA, Caputo D, Sala S, Judica E, Stroman PW, Filippi M. (2008). Evidence for enhanced functional activity of cervical cord in relapsing multiple sclerosis. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine 59 (5): 1035–42.
- ↑ Cruz LC, Domingues RC, Gasparetto EL (June 2009). Diffusion tensor imaging of the cervical spinal cord of patients with relapsing-remising multiple sclerosis: a study of 41 cases. Arq Neuropsiquiatr 67 (2B): 391–5.
- ↑ Agosta F, Absinta M, Sormani MP, et al. (August 2007). In vivo assessment of cervical cord damage in MS patients: a longitudinal diffusion tensor MRI study. Brain 130 (Pt 8): 2211–9.
- ↑ Gilmore C, Geurts J, Evangelou N, et al. (October 2008). Spinal cord grey matter lesions in multiple sclerosis detected by post-mortem high field MR imaging. Multiple Sclerosis 15 (2): 180–8.
- ↑ Pueyo V, Martin J, Fernandez J, Almarcegui C, Ara J, Egea C, Pablo L, Honrubia F. (2008). Axonal loss in the retinal nerve fiber layer in patients with multiple sclerosis. Multiple sclerosis (Houndmills, Basingstoke, England) 14 (5): 609–14.
- ↑ Zaveri MS, Conger A, Salter A, Frohman TC, Galetta SL, Markowitz CE, Jacobs DA, Cutter GR, Ying GS, Maguire MG, Calabresi PA, Balcer LJ, Frohman EM. (2008). Retinal Imaging by Laser Polarimetry and Optical Coherence Tomography Evidence of Axonal Degeneration in Multiple Sclerosis. Archives of neurology 65 (7): 924–8.
- ↑ Sepulcre J, Murie-Fernandez M, Salinas-Alaman A, García-Layana A, Bejarano B, Villoslada P (May 2007). Diagnostic accuracy of retinal abnormalities in predicting disease activity in MS. Neurology 68 (18): 1488–94.
- ↑ Naismith RT, Tutlam NT, Xu J, et al. (March 2009). Optical coherence tomography differs in neuromyelitis optica compared with multiple sclerosis. Neurology 72 (12): 1077–82.
- ↑ "eye, human."Encyclopædia Britannica. 2008. Encyclopædia Britannica 2006 Ultimate Reference Suite DVD
- ↑ Frohman EM, Fujimoto JG, Frohman TC, Calabresi PA, Cutter G, Balcer LJ (December 2008). Optical coherence tomography: a window into the mechanisms of multiple sclerosis. Nat Clin Pract Neurol 4 (12): 664–75.
- ↑ Lucarelli MJ, Pepose JS, Arnold AC, Foos RY (November 1991). Immunopathologic features of retinal lesions in multiple sclerosis. Ophthalmology 98 (11): 1652–6.
- ↑ Kerrison JB, Flynn T, Green WR (1994). Retinal pathologic changes in multiple sclerosis. Retina (Philadelphia, Pa.) 14 (5): 445–51.
- ↑ Gugleta K, Kochkorov A, Kavroulaki D, et al. (April 2009). Retinal vessels in patients with multiple sclerosis: baseline diameter and response to flicker light stimulation. Klin Monatsbl Augenheilkd 226 (4): 272–5.
- ↑ Kochkorov A, Gugleta K, Kavroulaki D, et al. (April 2009). Rigidity of retinal vessels in patients with multiple sclerosis. Klin Monatsbl Augenheilkd 226 (4): 276–9.
- ↑ Huizinga R, Gerritsen W, Heijmans N, Amor S (September 2008). Axonal loss and gray matter pathology as a direct result of autoimmunity to neurofilaments. Neurobiol Dis. 32 (3): 461–70.
- ↑ Sobottka B, Harrer MD, Ziegler U, et al. (September 2009). Collateral Bystander Damage by Myelin-Directed CD8+ T Cells Causes Axonal Loss. Am. J. Pathol. 175 (3): 1160–6.
- ↑ Filippi M, Bozzali M, Rovaris M, Gonen O, Kesavadas C, Ghezzi A, Martinelli V, Grossman R, Scotti G, Comi G, Falini A (2003). Evidence for widespread axonal damage at the earliest clinical stage of multiple sclerosis. Brain 126 (Pt 2): 433–7.
- ↑ Neuer Diagnose-Ansatz zur Früherkennung von MS
- ↑ Mostert JP, Blaauw Y, Koch MW, Kuiper AJ, Hoogduin JM, De Keyser J (2008). Reproducibility over a 1-month period of 1H-MR spectroscopic imaging NAA/Cr ratios in clinically stable multiple sclerosis patients. Eur Radiol 18 (8): 1736–40.
- ↑ Charles M. Poser, The peripheral nervous system in multiple sclerosis: A review and pathogenetic hypothesis, http://dx.doi.org/10.1016/0022-510X(87)90262-0
- ↑ Compston A, Coles A (October 2008). Multiple sclerosis. Lancet 372 (9648): 1502–17.
- ↑ (December 2009). Multiple sclerosis: distribution of inflammatory cells in newly forming lesions. Annals of neurology 66 (6): 739–53.
- ↑ van Walderveen MA; Kamphorst W; Scheltens P; van Waesberghe JH; Ravid R; Valk J; Polman CH; Barkhof F, Histopathologic correlate of hypointense lesions on T1-weighted spin-echo MRI in multiple sclerosis. [2]
- ↑ Antonov SM, Kalinina NI, Kurchavyj GG, Magazanik LG, Shupliakov OV, Vesselkin NP (February 1990). Identification of two types of excitatory monosynaptic inputs in frog spinal motoneurones. Neuroscience letters 109 (1–2): 82–7.
- ↑ Alireza Minagar and J Steven Alexander, Blood–brain barrier disruption in multiple sclerosis [3]
- ↑ Soon D, Tozer DJ, Altmann DR, Tofts PS, Miller DH (2007). Quantification of subtle blood–brain barrier disruption in non-enhancing lesions in multiple sclerosis: a study of disease and lesion subtypes. Multiple Sclerosis 13 (7): 884–94.
- ↑ Minagar A, Jy W, Jimenez JJ, Alexander JS (2006). Multiple sclerosis as a vascular disease. Neurol. Res. 28 (3): 230–5.
- ↑ 64.0 64.1 Gray E, Thomas TL, Betmouni S, Scolding N, Love S (September 2008). Elevated matrix metalloproteinase-9 and degradation of perineuronal nets in cerebrocortical multiple sclerosis plaques. J Neuropathol Exp Neurol. 67 (9): 888–99.
- ↑ 65.0 65.1 65.2 van der Valk P, Amor S (June 2009). Preactive lesions in multiple sclerosis. Curr. Opin. Neurol. 22 (3): 207–13.
- ↑ 66.0 66.1 Werring DJ, Brassat D, Droogan AG, et al. (August 2000). The pathogenesis of lesions and normal-appearing white matter changes in multiple sclerosis: a serial diffusion MRI study. Brain 123 (8): 1667–76.
- ↑ 67.0 67.1 Allen et al. (2001). Pathological abnormalities in the normal-appearing white matter in multiple sclerosis. Neurol Sci 22 (2): 141–4.
- ↑ Shinohara RT, Crainiceanu CM, Caffo BS, Gaitán MI, Reich DS (May 2011). Population-Wide Principal Component-Based Quantification of Blood-Brain-Barrier Dynamics in Multiple Sclerosis. NeuroImage 57 (4): 1430–46.
- ↑ Pan W, Hsuchou H, Yu C, Kastin AJ (2008). Permeation of blood-borne IL15 across the blood–brain barrier and the effect of LPS. J. Neurochem. 106 (1): 313–9.
- ↑ Reijerkerk A, Kooij G, van der Pol SM, Leyen T, van Het Hof B, Couraud PO, Vivien D, Dijkstra CD, de Vries HE. (2008). Tissue-type plasminogen activator is a regulator of monocyte diapedesis through the brain endothelial barrier. Journal of immunology (Baltimore, Md. : 1950) 181 (5): 3567–74.
- ↑ Malik M, Chen YY, Kienzle MF, Tomkowicz BE, Collman RG, Ptasznik A (October 2008). Monocyte migration and LFA-1 mediated attachment to brain microvascular endothelia is regulated by SDF-1α through Lyn kinase. J Immunol. 181 (7): 4632–7.
- ↑ Petry KG, Boiziau C, Dousset V, Brochet B (2007). Magnetic resonance imaging of human brain macrophage infiltration. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics 4 (3): 434–42.
- ↑ Boz C, Ozmenoglu M, Velioglu S, et al. (February 2006). Matrix metalloproteinase-9 (MMP-9) and tissue inhibitor of matrix metalloproteinase (TIMP-1) in patients with relapsing-remitting multiple sclerosis treated with interferon beta. Clin Neurol Neurosurg. 108 (2): 124–8.
- ↑ Waubant E (2006). Biomarkers indicative of blood–brain barrier disruption in multiple sclerosis. Dis. Markers 22 (4): 235–44.
- ↑ 75.0 75.1 eMedicine neuro/228
- ↑ Elovaara I, Ukkonen M, Leppäkynnäs M, et al. (April 2000). Adhesion molecules in multiple sclerosis: relation to subtypes of disease and methylprednisolone therapy. Arch. Neurol. 57 (4): 546–51.
- ↑ Alexandre Prat, Nicole Beaulieu, Sylvain-Jacques Desjardins, New Therapeutic Target For Treatment Of Multiple Sclerosis, Jan. 2008
- ↑ McCandless EE, Piccio L, Woerner BM, et al. (March 2008). Pathological Expression of CXCL12 at the Blood-Brain Barrier Correlates with Severity of Multiple Sclerosis. Am J Pathol. 172 (3): 799–808.
- ↑ Moll NM, Cossoy MB, Fisher E, et al. (January 2009). Imaging correlates of leukocyte accumulation and CXCR4/CXCR12 in multiple sclerosis. Arch. Neurol. 66 (1): 44–53.
- ↑ Michałowska-Wender G, Losy J, Biernacka-Łukanty J, Wender M (2008). Impact of methylprednisolone treatment on the expression of macrophage inflammatory protein 3alpha and B lymphocyte chemoattractant in serum of multiple sclerosis patients. Pharmacol Rep. 60 (4): 549–54.
- ↑ Steinman L (May 2009). A molecular trio in relapse and remission in multiple sclerosis. Nat. Rev. Immunol. 9 (6): 440–7.
- ↑ Waubant E (2006). Biomarkers indicative of blood–brain barrier disruption in multiple sclerosis. Disease Markers 22 (4): 235–44.
- ↑ Leech S, Kirk J, Plumb J, McQuaid S (2007). Persistent endothelial abnormalities and blood–brain barrier leak in primary and secondary progressive multiple sclerosis. Neuropathol. Appl. Neurobiol. 33 (1): 86–98.
- ↑ Kean R, Spitsin S, Mikheeva T, Scott G, Hooper D (2000). The peroxynitrite scavenger uric acid prevents inflammatory cell invasion into the central nervous system in experimental allergic encephalomyelitis through maintenance of blood-central nervous system barrier integrity. J. Immunol. 165 (11): 6511–8.
- ↑ Rentzos M, Nikolaou C, Anagnostouli M, Rombos A, Tsakanikas K, Economou M, Dimitrakopoulos A, Karouli M, Vassilopoulos D (2006). Serum uric acid and multiple sclerosis. Clinical neurology and neurosurgery 108 (6): 527–31.
- ↑ van Horssen J, Brink BP, de Vries HE, van der Valk P, Bø L (April 2007). The blood–brain barrier in cortical multiple sclerosis lesions. J Neuropathol Exp Neurol. 66 (4): 321–8.
- ↑ Guerrero AL, Martín-Polo J, Laherrán E, et al. (April 2008). Variation of serum uric acid levels in multiple sclerosis during relapses and immunomodulatory treatment. Eur J Neurol. 15 (4): 394–7.
- ↑ Laule C, Vavasour IM, Kolind SH, et al. (2007). Long T(2) water in multiple sclerosis: What else can we learn from multi-echo T(2) relaxation?. J. Neurol. 254 (11): 1579–87.
- ↑ Zhang Y, Zabad R, Wei X, Metz LM, Hill MD, Mitchell JR (2007). Deep grey matter 'black T2' on 3 tesla magnetic resonance imaging correlates with disability in multiple sclerosis. Multiple Sclerosis 13 (7): 880–3.
- ↑ Holley JE, Newcombe J, Winyard PG, Gutowski NJ (2007). Peroxiredoxin V in multiple sclerosis lesions: predominant expression by astrocytes. Multiple Sclerosis 13 (8): 955–61.
- ↑ Otaduy MC, Callegaro D, Bacheschi LA, Leite CC (December 2006). Correlation of magnetization transfer and diffusion magnetic resonance imaging in multiple sclerosis. Multiple sclerosis 12 (6): 754–9.
- ↑ Nelson F, Poonawalla A, Hou P, Wolinsky J, Narayana P (November 2008). 3D MPRAGE Improves Classification of Cortical Lesions in Multiple Sclerosis. Multiple Sclerosis 14 (9): 1214–9.
- ↑ Haacke EM, Makki M, Ge Y, et al. (March 2009). Characterizing iron deposition in multiple sclerosis lesions using susceptibility weighted imaging. J Magn Reson Imaging 29 (3): 537–44.
- ↑ Zhang J, Tong L, Wang L, Li N (2008). Texture analysis of multiple sclerosis: a comparative study. Magnetic resonance imaging 26 (8): 1160–6.
- ↑ Seewann A, Vrenken H, van der Valk P, et al. (May 2009). Diffusely abnormal white matter in chronic multiple sclerosis: imaging and histopathologic analysis. Arch. Neurol. 66 (5): 601–9.
- ↑ (March 2010). Diffusely abnormal white matter in progressive multiple sclerosis: in vivo quantitative MR imaging characterization and comparison between disease types. AJNR. American journal of neuroradiology 31 (3): 541–8.
- ↑ Kooi EJ, van Horssen J, Witte ME, et al. (June 2009). Abundant extracellular myelin in the meninges of patients with multiple sclerosis. Neuropathol. Appl. Neurobiol. 35 (3): 283–95.
- ↑ A.M. Saindane, M. Law, Y. Ge, G. Johnson, J.S. Babb and R.I. Grossman, Correlation of Diffusion Tensor and Dynamic Perfusion MR Imaging Metrics in Normal-Appearing Corpus Callosum: Support for Primary Hypoperfusion in Multiple Sclerosis, American Journal of Neuroradiology 28:767-772, April 2007 [4]
- ↑ (October 1998). The multiple sclerosis lesion: initiated by a localized hypoperfusion in a central nervous system where mechanisms allowing leukocyte infiltration are readily upregulated?. Medical hypotheses 51 (4): 299–303.
- ↑ Matilde Inglese, Sumita Adhya, Glyn Johnson, James S Babb, Laura Miles, Hina Jaggi, Joseph Herbert, and Robert Grossman, Perfusion magnetic resonance imaging correlates of neuropsychological impairment in multiple sclerosis, DOI:10.1038/sj.jcbfm.9600504 [5]
- ↑ Sumita Adhya, MS, Glyn Johnson, PhD, Joseph Herbert, MD,* Hina Jaggi, MS, James S. Babb, PhD, Robert I. Grossman, MD, and Matilde Inglese, MD, PhD, Pattern of Hemodynamic Impairment in Multiple Sclerosis: Dynamic Susceptibility Contrast Perfusion MR Imaging at 3.0 T, DOI:10.1016/j.neuroimage.2006.08.008 .
- ↑ 102.0 102.1 Varga AW, Johnson G, Babb JS, Herbert J, Grossman RI, Inglese M (July 2009). White Matter Hemodynamic Abnormalities precede Sub-cortical Gray Matter Changes in Multiple Sclerosis. J. Neurol. Sci. 282 (1–2): 28–33.
- ↑ 103.0 103.1 (October 2008). Hypoperfusion of the cerebral white matter in multiple sclerosis: possible mechanisms and pathophysiological significance. Journal of Cerebral Blood Flow and Metabolism 28 (10): 1645–51.
- ↑ Matilde Inglese, Sumita Adhya, Glyn Johnson, James S Babb, Laura Miles, Hina Jaggi, Joseph Herbert and Robert I Grossman, Perfusion magnetic resonance imaging correlates of neuropsychological impairment in multiple sclerosis, DOI:10.1038/sj.jcbfm.9600504 [6]
- ↑ (June 2004). Microvascular abnormality in relapsing-remitting multiple sclerosis: perfusion MR imaging findings in normal-appearing white matter. Radiology 231 (3): 645–52.
- ↑ (February 1988). Perivascular iron deposition and other vascular damage in multiple sclerosis. Journal of neurology, neurosurgery, and psychiatry 51 (2): 260–5.
- ↑ (December 2009). Anomalous venous blood flow and iron deposition in multiple sclerosis. Journal of Cerebral Blood Flow and Metabolism 29 (12): 1867–78.
- ↑ Bizzozero OA, DeJesus G, Callahan K, Pastuszyn A. (2005). Elevated protein carbonylation in the brain white matter and gray matter of patients with multiple sclerosis. Journal of neuroscience research 81 (5): 687–95.
- ↑ Clements RJ, McDonough J, Freeman EJ. (2008). Distribution of parvalbumin and calretinin immunoreactive interneurons in motor cortex from multiple sclerosis post-mortem tissue. Experimental brain research. Experimentelle Hirnforschung. Experimentation cerebrale 187 (3): 459–65.
- ↑ Lukas Haider et al. Oxidative damage in multiple sclerosis lesions, Brain Advance Access published June 7, 2011, DOI:10.1093/brain/awr128 [7]
- ↑ Thomas Zeis,Ursula Graumann,Richard Reynolds, Nicole Schaeren-Wiemers (Jan 2008). Normal-appearing white matter in multiple sclerosis is in a subtle balance between inflammation and neuroprotection. Brain 131 (4): 288–303.
- ↑ 112.0 112.1 (April 2004). Relapsing and remitting multiple sclerosis: pathology of the newly forming lesion. Annals of neurology 55 (4): 458–68.
- ↑ Phuttharak W, Galassi W, Laopaiboon V, Laopaiboon M, Hesselink JR (2007). Abnormal diffusivity of normal appearing brain tissue in multiple sclerosis: a diffusion-weighted MR imaging study. J Med Assoc Thai 90 (12): 2689–94.
- ↑ Nicholas AP, Sambandam T, Echols JD, Tourtellotte WW. (2004). Increased citrullinated glial fibrillary acidic protein in secondary progressive multiple sclerosis. The Journal of Comparative Neurology 473 (1): 128–36.
- ↑ Wheeler D, Bandaru VV, Calabresi PA, Nath A, Haughey NJ (November 2008). A defect of sphingolipid metabolism modifies the properties of normal appearing white matter in multiple sclerosis. Brain 131 (Pt 11): 3092–102.
- ↑ Too Much Of A Charge-Switching Enzyme Causes Symptoms Of Multiple Sclerosis And Related Disorders In Mouse Models http://www.medicalnewstoday.com/articles/128393.php
- ↑ De Keyser J, Steen C, Mostert JP, Koch MW. (2008). Hypoperfusion of the cerebral white matter in multiple sclerosis: possible mechanisms and pathophysiological significance. Journal of Cerebral Blood Flow and Metabolism 28 (10): 1645–51.
- ↑ Filippi M, Rocca MA, Martino G, Horsfield MA, Comi G (June 1998). Magnetization transfer changes in the normal appearing white matter precede the appearance of enhancing lesions in patients with multiple sclerosis. Ann Neurol. 43 (6): 809–14.
- ↑ Cercignani M, Iannucci G, Rocca MA, Comi G, Horsfield MA, Filippi M (March 2000). Pathologic damage in MS assessed by diffusion-weighted and magnetization transfer MRI. Neurology 54 (5): 1139–44.
- ↑ van Waesberghe JH, Kamphorst W, De Groot CJ, et al. (November 1999). Axonal loss in multiple sclerosis lesions: magnetic resonance imaging insights into substrates of disability. Ann Neurol. 46 (5): 747–54.
- ↑ Tait AR, Straus SK (August 2008). Phosphorylation of U24 from Human Herpes Virus type 6 (HHV-6) and its potential role in mimicking myelin basic protein (MBP) in multiple sclerosis. FEBS Letters 582 (18): 2685–8.
- ↑ Fisher E, Lee JC, Nakamura K, Rudick RA (September 2008). Gray matter atrophy in multiple sclerosis: a longitudinal study. Ann Neurol. 64 (3): 255–65.
- ↑ Zivadinov R, Zorzon M, Weinstock-Guttman B, et al. (June 2009). Epstein-Barr virus is associated with grey matter atrophy in multiple sclerosis. J. Neurol. Neurosurg. Psychiatr. 80 (6): 620–5.
- ↑ Willis SN, Stadelmann C, Rodig SJ, et al. (July 2009). Epstein–Barr virus infection is not a characteristic feature of multiple sclerosis brain. Brain 132 (Pt 12): 3318–28.
- ↑ Vercellino M, Masera S, Lorenzatti M, et al. (May 2009). Demyelination, inflammation, and neurodegeneration in multiple sclerosis deep gray matter. J. Neuropathol. Exp. Neurol. 68 (5): 489–502.
- ↑ Ge Y, Jensen JH, Lu H, et al. (October 2007). Quantitative assessment of iron accumulation in the deep gray matter of multiple sclerosis by magnetic field correlation imaging. AJNR Am J Neuroradiol 28 (9): 1639–44.
- ↑ (October 2010). Pathological basis of diffusely abnormal white matter: insights from magnetic resonance imaging and histology. Multiple sclerosis (Houndmills, Basingstoke, England) 17 (2): 144–50.
- ↑ Seewann A, Vrenken H, van der Valk P, et al. (May 2009). Diffusely abnormal white matter in chronic multiple sclerosis: imaging and histopathologic analysis. Arch. Neurol. 66 (5): 601–9.
- ↑ Vos CM, Geurts JJ, Montagne L, et al. (December 2005). Blood-brain barrier alterations in both focal and diffuse abnormalities on postmortem MRI in multiple sclerosis. Neurobiol. Dis. 20 (3): 953–60.
- ↑ Lassmann H (July 2005). Multiple sclerosis pathology: evolution of pathogenetic concepts. Brain Pathology 15 (3): 217–22.Template:Vn
- ↑ Putnam, T.J. (1937) Evidence of vascular occlusion in multiple sclerosis
- ↑ (October 1986). Damaging venous reflux into the skull or spine: relevance to multiple sclerosis. Medical hypotheses 21 (2): 141–8.
- ↑ Walter U, Wagner S, Horowski S, Benecke R, Zettl UK (September 2009). Transcranial brain sonography findings predict disease progression in multiple sclerosis. Neurology 73 (13): 1010–7.
- ↑ Leech S, Kirk J, Plumb J, McQuaid S (February 2007). Persistent endothelial abnormalities and blood–brain barrier leak in primary and secondary progressive multiple sclerosis. Neuropathol. Appl. Neurobiol. 33 (1): 86–98.
- ↑ Ge Y, Zohrabian VM, Grossman RI. (2008). 7T MRI: New Vision of Microvascular Abnormalities in Multiple Sclerosis. Archives of neurology 65 (6): 812–6.
- ↑ (2004). Normal-appearing White and Grey Matter Damage in Multiple Sclerosis. Book review. AJRN.
- ↑ (March 2010). Wedge-shaped medullary lesions in multiple sclerosis. Journal of the neurological sciences 290 (1–2): 190–3.
- ↑ 138.0 138.1 Zamboni P, Galeotti R, Menegatti E, et al. (April 2009). Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J. Neurol. Neurosurg. Psychiatr. 80 (4): 392–9.
- ↑ 139.0 139.1 Khan O, Filippi M, Freedman MS, et al. (March 2010). Chronic cerebrospinal venous insufficiency and multiple sclerosis. Ann. Neurol. 67 (3): 286–90.
- ↑ Bryce Weir (2010). MS, A vascular ethiology?. Can. J. Neurol. Sci. 2010; 37: 745-757.
- ↑ Bartolomei I. et al (April 2010). Haemodynamic patterns in chronic cereblrospinal venous insufficiency in multiple sclerosis. Correlation of symptoms at onset and clinical course. Int Angiol 29 (2): 183–8.
- ↑ Zamboni P, Menegatti E, Bartolomei I, et al. (November 2007). Intracranial venous haemodynamics in multiple sclerosis. Curr Neurovasc Res. 4 (4): 252–8.
- ↑ Zamboni P, Galeotti R, Menegatti E, et al. (April 2009). Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J. Neurol. Neurosurg. Psychiatr. 80 (4): 392–9.
- ↑ Lee AB, Laredo J, Neville R (April 2010). Embryological background of truncular venous malformation in the extracranial venous pathways as the cause of chronic cerebro spinal venous insufficiency. Int Angiol 29 (2): 95–108.
- ↑ Al-Omari MH, Rousan LA (April 2010). Internal jugular vein morphology and hemodynamics in patients with multiple sclerosis. Int Angiol 29 (2): 115–20.
- ↑ Krogias C, Schröder A, Wiendl H, Hohlfeld R, Gold R (April 2010). ["Chronic cerebrospinal venous insufficiency" and multiple sclerosis : Critical analysis and first observation in an unselected cohort of MS patients.]. Nervenarzt 81 (6): 740–6.
- ↑ Doepp F, Paul F, Valdueza JM, Schmierer K, Schreiber SJ (August 2010). No cerebrocervical venous congestion in patients with multiple sclerosis. Ann. Neurol. 68 (2): 173–83.
- ↑ DOI:10.1002/ana.22132
This citation will be automatically completed in the next few minutes. You can jump the queue or expand by hand - ↑ Damadian RV, Chu D. The possible role of cranio-cervical trauma and abnormal CSF hydrodynamics in the genesis of multiple sclerosis, 2011, [8]
- ↑ Zamboni et al. CSF dynamics and brain volume in multiple sclerosis are associated with extracranial venous flow anomalies, 2010 [9]
- ↑ Raymond V. Damadian and David Chu, The Possible Role of Cranio-Cervical Trauma and Abnormal CSF Hydrodynamics in the Genesis of Multiple Sclerosis [10][11][12]
- ↑ Haufschild T, Shaw SG, Kesselring J, Flammer J. Increased endothelin-1 plasma levels in patients with multiple sclerosis. J Neuroophthalmol. 2001 Mar;21(1):37-8.
- ↑ Kanabrocki EL, Ryan MD, Hermida RC, et al. (2008). Uric acid and renal function in multiple sclerosis. Clin Ter 159 (1): 35–40.
- ↑ Yang L, Anderson DE, Kuchroo J, Hafler DA (2008). Lack of TIM-3 Immunoregulation in Multiple Sclerosis. J. Immunol. 180 (7): 4409–4414.
- ↑ Malmeström C, Lycke J, Haghighi S, Andersen O, Carlsson L, Wadenvik H, Olsson B. (2008). Relapses in multiple sclerosis are associated with increased CD8(+) T-cell mediated cytotoxicity in CSF. J Neuroimmunol. 196 (Apr.5): 35–40.
- ↑ Satoh J. (2008). Molecular biomarkers for prediction of multiple sclerosis relapse. Nippon Rinsho 66 (6): 1103–11.
- ↑ Sheremata WA, Jy W, Horstman LL, Ahn YS, Alexander JS, Minagar A. (2008). Evidence of platelet activation in multiple sclerosis. J Neuroinflammation 5: 27.
- ↑ Astier AL (2008). T-cell regulation by CD46 and its relevance in multiple sclerosis. Immunology 124 (2): 149–54.
- ↑ Kanabrocki EL, Ryan MD, Lathers D, Achille N, Young MR, Cauteren JV, Foley S, Johnson MC, Friedman NC, Siegel G, Nemchausky BA. (2007). Circadian distribution of serum cytokines in multiple sclerosis. Clin. Ter. 158 (2): 157–62.
- ↑ Rentzos M, Nikolaou C, Rombos A, Evangelopoulos ME, Kararizou E, Koutsis G, Zoga M, Dimitrakopoulos A, Tsoutsou A, Sfangos C. (2008). Effect of treatment with methylprednisolone on the serum levels of IL-12, IL-10 and CCL2 chemokine in patients with multiple sclerosis in relapse. Clinical neurology and neurosurgery 110 (10): 992–6.
- ↑ Scarisbrick IA, Linbo R, Vandell AG, Keegan M, Blaber SI, Blaber M, Sneve D, Lucchinetti CF, Rodriguez M, Diamandis EP. (2008). Kallikreins are associated with secondary progressive multiple sclerosis and promote neurodegeneration. Biological chemistry 389 (6): 739–45.
- ↑ New Control System Of The Body Discovered - Important Modulator Of Immune Cell Entry Into The Brain - Perhaps New Target For The Therapy, Dr. Ulf Schulze-Topphoff, Prof. Orhan Aktas, and Professor Frauke Zipp (Cecilie Vogt-Clinic, Charité - Universitätsmedizin Berlin, Max Delbrück Center for Molecular Medicine (MDC) Berlin-Buch and NeuroCure Research Center) [13]
- ↑ Schulze-Topphoff U, Prat A, Prozorovski T, et al. (July 2009). Activation of kinin receptor B1 limits encephalitogenic T lymphocyte recruitment to the central nervous system. Nat. Med. 15 (7): 788–93.
- ↑ Rinta S, Kuusisto H, Raunio M, et al. (October 2008). Apoptosis-related molecules in blood in multiple sclerosis. J Neuroimmunol. 205 (1–2): 135–41.
- ↑ Kuenz B, Lutterotti A, Ehling R, et al. (2008). Cerebrospinal Fluid B Cells Correlate with Early Brain Inflammation in Multiple Sclerosis. PLoS ONE 3 (7): e2559.
- ↑ Chiasserini D, Di Filippo M, Candeliere A, Susta F, Orvietani PL, Calabresi P, Binaglia L, Sarchielli P. (2008). CSF proteome analysis in multiple sclerosis patients by two-dimensional electrophoresis. European Journal of Neurology 15 (9): 998–1001.
- ↑ Frisullo G, Nociti V, Iorio R, et al. (October 2008). The persistency of high levels of pSTAT3 expression in circulating CD4+ T cells from CIS patients favors the early conversion to clinically defined multiple sclerosis. J Neuroimmunol. 205 (1–2): 126–34.
- ↑ Proceedings of the National Academy of sciences, complementary information [14]
- ↑ 169.0 169.1 Quintana FJ, Farez MF, Viglietta V, et al. (December 2008). Antigen microarrays identify unique serum autoantibody signatures in clinical and pathologic subtypes of multiple sclerosis. Proc. Natl. Acad. Sci. U.S.A. 105 (48): 18889–94.
- ↑ Villar LM, Masterman T, Casanova B, et al. (June 2009). CSF oligoclonal band patterns reveal disease heterogeneity in multiple sclerosis. J. Neuroimmunol. 211 (1–2): 101–4.
- ↑ Rajneesh Srivastava, M.Sc et al. "Potassium Channel KIR4.1 as an Immune Target in Multiple Sclerosis", New England Journal of medicine
- ↑ Plumb J, McQuaid S, Mirakhur M, Kirk J (April 2002). Abnormal endothelial tight junctions in active lesions and normal-appearing white matter in multiple sclerosis. Brain Pathol. 12 (2): 154–69.
- ↑ Mancini, M, Cerebral circulation time in the evaluation of neurological diseases [15]
- ↑ Meng Law et al. Microvascular Abnormality in Relapsing-Remitting Multiple Sclerosis: Perfusion MR Imaging Findings in Normal-appearing White Matter [16]
- ↑ Sarchielli P, Greco L, Floridi A, Floridi A, Gallai V. (2003). Excitatory amino acids and multiple sclerosis: evidence from cerebrospinal fluid. Arch. Immunol. 60 (8): 1082–8.
- ↑ Stoop MP, Dekker LJ, Titulaer MK, et al. (2008). Multiple sclerosis-related proteins identified in cerebrospinal fluid by advanced mass spectrometry. Proteomics 8 (8): 1576–85.
- ↑ Sarchielli P, Di Filippo M, Ercolani MV, et al. (April 2008). Fibroblast growth factor-2 levels are elevated in the cerebrospinal fluid of multiple sclerosis patients. Neurosci Lett. 435 (3): 223–8.
- ↑ Huttner HB, Schellinger PD, Struffert T, et al. (July 2009). MRI criteria in MS patients with negative and positive oligoclonal bands: equal fulfillment of Barkhof's criteria but different lesion patterns. J. Neurol. 256 (7): 1121–5.
- ↑ Sotelo J, Martínez-Palomo A, Ordoñez G, Pineda B. (2008). Varicella-zoster virus in cerebrospinal fluid at relapses of multiple sclerosis. Ann Neurol. 63 (3): 303–11.
- ↑ von Büdingen HC, Harrer MD, Kuenzle S, Meier M, Goebels N (July 2008). Clonally expanded plasma cells in the cerebrospinal fluid of MS patients produce myelin-specific antibodies. Eur J Immunol. 38 (7): 2014–23.
- ↑ Vincze O, Oláh J, Zádori D, Klivényi P, Vécsei L, Ovádi J (May 2011). A new myelin protein, TPPP/p25, reduced in demyelinated lesions is enriched in cerebrospinal fluid of multiple sclerosis. Biochem. Biophys. Res. Commun. 409 (1): 137–41.
- ↑ Cozzone, Zaaraoui and Ranjeva, "Distribution of Brain Sodium Accumulation Correlates with Disability in Multiple Sclerosis–A Cross-Sectional 23Na MR Imaging Study." Radiological Society of North America
- ↑ Satoh J. (2008). Molecular biomarkers for prediction of multiple sclerosis relapse. Nippon Rinsho 66 (6): 1103–11.
- ↑ García-Barragán N, Villar LM, Espiño M, Sádaba MC, González-Porqué P, Alvarez-Cermeño JC (March 2009). Multiple sclerosis patients with anti-lipid oligoclonal IgM show early favourable response to immunomodulatory treatment. Eur. J. Neurol. 16 (3): 380–5.
- ↑ Hagman S, Raunio M, Rossi M, Dastidar P, Elovaara I (May 2011). Disease-associated inflammatory biomarker profiles in blood in different subtypes of multiple sclerosis: Prospective clinical and MRI follow-up study. Journal of Neuroimmunology 234 (1–2): 141–7.
- ↑ Leussink VI, Lehmann HC, Meyer Zu Hörste G, Hartung HP, Stüve O, Kieseier BC (September 2008). Rituximab induces clinical stabilization in a patient with fulminant multiple sclerosis not responding to natalizumab : Evidence for disease heterogeneity. J Neurology 255 (9): 1436–8.
- ↑ Gold R, Linington C (July 2002). Devic's disease: bridging the gap between laboratory and clinic. Brain 125 (Pt 7): 1425–7.
- ↑ Holmes, Nick Part 1B Pathology: Lecture 11 - The Complement System. URL accessed on 2006-05-10.
- ↑ Lucchinetti, Claudia, Wolfgang Brück, Joseph Parisi, Bernd Scheithauer, Moses Rodriguez and Hans Lassmann (December 1999). A quantitative analysis of oligodendrocytes in multiple sclerosis lesions - A study of 113 cases. Brain 122 (12): 2279–2295.
- ↑ Kale N, Pittock SJ, Lennon VA, et al. (October 2009). Humoral pattern II multiple sclerosis pathology not associated with neuromyelitis Optica IgG. Arch. Neurol. 66 (10): 1298–9.
- ↑ Michael H. Barnett, MBBS and John W. Prineas, MBBS (2004). Relapsing and Remitting Multiple Sclerosis: Pathology of the Newly Forming Lesion. Ann Neurol 55 (1): 458–468.
- ↑ Breij EC, Brink BP, Veerhuis R, et al. (2008). Homogeneity of active demyelinating lesions in established multiple sclerosis. Ann Neurol 63 (1): 16–25.
- ↑ Mahad D, Ziabreva I, Lassmann H, Turnbull D. (2008). Mitochondrial defects in acute multiple sclerosis lesions. Brain : a journal of neurology 131 (Pt 7): 1722–35.
- ↑ Primary progressive multiple sclerosis
- ↑ (Article in Spanish) Estudio longitudinal mediante imagen de resonancia magnética (RM) del efecto de la azatioprina [17]
- ↑ The Mystery of the Multiple Sclerosis Lesion, Frontiers Beyond the Decade of the Brain, Medscape [18]
- ↑ Smith SA, Farrell JA, Jones CK, Reich DS, Calabresi PA, van Zijl PC (October 2006). Pulsed magnetization transfer imaging with body coil transmission at 3 Tesla: feasibility and application. Magn Reson Med 56 (4): 866–75.
- ↑ Goldberg-Zimring D, Mewes AU, Maddah M, Warfield SK (2005). Diffusion tensor magnetic resonance imaging in multiple sclerosis. J Neuroimaging 15 (4 Suppl): 68S–81S.
- ↑ New imaging technique allows doctors to ‘see’ molecular activity
- ↑ Cepok S, Jacobsen M, Schock S, et al. (November 2001). Patterns of cerebrospinal fluid pathology correlate with disease progression in multiple sclerosis. Brain 124 (Pt 11): 2169–76.
- ↑ Cepok S, Jacobsen M, Schock S, et al. (November 2001). Patterns of cerebrospinal fluid pathology correlate with disease progression in multiple sclerosis. Brain 124 (Pt 11): 2169–76.
- ↑ Pittock SJ, Reindl M, Achenbach S, et al. (January 2007). Myelin oligodendrocyte glycoprotein antibodies in pathologically proven multiple sclerosis: frequency, stability and clinicopathologic correlations. Multiple Sclerosis 13 (1): 7–16.
- ↑ Belogurov AA, Kurkova IN, Friboulet A, et al. (January 2008). Recognition and degradation of myelin basic protein peptides by serum autoantibodies: novel biomarker for multiple sclerosis. J Immunol. 180 (2): 1258–67.
- ↑ Early research into a treatment for progressive MS
- ↑ Fernández O, Fernández V, Mayorga C, et al. (December 2005). HLA class II and response to interferon-beta in multiple sclerosis. Acta Neurol Scand. 112 (6): 391–4.
- ↑ van Baarsen LG, Vosslamber S, Tijssen M, et al. (2008). Pharmacogenomics of Interferon-β Therapy in Multiple Sclerosis: Baseline IFN Signature Determines Pharmacological Differences between Patients. PLoS ONE 3 (4): e1927.
- ↑ Wiesemann E, Deb M, Hemmer B, Radeke HH, Windhagen A. (2008). Early identification of interferon-beta responders by ex vivo testing in patients with multiple sclerosis. Clinical immunology (Orlando, Fla.) 128 (3): 306–13.
- ↑ Axtell RC et a. T helper type 1 and 17 cells determine efficacy of interferon-beta in multiple sclerosis and experimental encephalomyelitis, PMID 20348925
- ↑ Carrieri PB, Ladogana P, Di Spigna G, et al. (2008). Interleukin-10 and interleukin-12 modulation in patients with relapsing-remitting multiple sclerosis on therapy with interferon-beta 1a: differences in responders and non responders. Immunopharmacol Immunotoxicol. 30 (4): 1–9.
- ↑ Wilner AN, Goodman (March 2000). Some MS patients have "Dramatic" responses to Plasma Exchange. Neurology Reviews 8 (3).
- ↑ Patients' Multiple Sclerosis Lesion Type Dictates Effective Treatment
- ↑ Bitsch A, Brück W (2002). Differentiation of multiple sclerosis subtypes: implications for treatment. CNS Drugs 16 (6): 405–18.
- ↑ Debouverie M, Moreau T, Lebrun C, Heinzlef O, Brudon F, Msihid J (November 2007). A longitudinal observational study of a cohort of patients with relapsing-remitting multiple sclerosis treated with glatiramer acetate. Eur J Neurol. 14 (11): 1266–74.
- ↑ Carrá A, Onaha P, Luetic G, et al. (2008). Therapeutic outcome 3 years after switching of immunomodulatory therapies in patients with relapsing-remitting multiple sclerosis in Argentina. Eur. J. Neurol. 15 (4): 386–93.
- ↑ Gajofatto A, Bacchetti P, Grimes B, High A, Waubant E (October 2008). Switching first-line disease-modifying therapy after failure: impact on the course of relapsing-remitting multiple sclerosis. Multiple sclerosis 15 (1): 50–8.
- ↑ Byun E, Caillier SJ, Montalban X, et al. (March 2008). Genome-wide pharmacogenomic analysis of the response to interferon beta therapy in multiple sclerosis. Arch. Neurol. 65 (3): 337–44.
- ↑ Vandenbroeck K, Matute C (May 2008). Pharmacogenomics of the response to IFN-beta in multiple sclerosis: ramifications from the first genome-wide screen. Pharmacogenomics 9 (5): 639–45.
- ↑ Frisullo G, Nociti V, Iorio R, et al. (December 2008). The persistency of high levels of pSTAT3 expression in circulating CD4+ T cells from CIS patients favors the early conversion to clinically defined multiple sclerosis. J Neuroimmunol. 205 (1-2): 126–34.
- ↑ Hakiki B, Goretti B, Portaccio E, Zipoli V, Amato MP. (2008). Subclinical MS: follow-up of four cases. European Journal of Neurology 15 (8): 858–61.
- ↑ Engell T (May 1989). A clinical patho-anatomical study of clinically silent multiple sclerosis. Acta Neurol. Scand. 79 (5): 428–30.
- ↑ Mews I, Bergmann M, Bunkowski S, Gullotta F, Brück W (April 1998). Oligodendrocyte and axon pathology in clinically silent multiple sclerosis lesions. Mult. Scler. 4 (2): 55–62.
- ↑ Lebrun C, Bensa C, Debouverie M, et al. (2008). Unexpected multiple sclerosis: follow-up of 30 patients with magnetic resonance imaging and clinical conversion profile. J Neurol Neurosurg Psychiatry 79 (2): 195–198.
External links[]
- The lesion project page
- MRI and CT of Multiple Sclerosis MedPix Image Database
Multiple sclerosis | |
|---|---|
| Signs and symptoms |
Ataxia · Depression · Diplopia · Dysarthria · Dysphagia · Fatigue · Incontinence · Neurological fatigue · Nystagmus · Optic neuritis · Pain |
| Diagnosis and evolution following |
McDonald criteria · EDSS |
| Investigation |
Pathophysiology · Experimental autoimmune encephalomyelitis |
| Therapies |
Interferon · Glatiramer acetate · Mitoxantrone · Natalizumab · Therapies under investigation |
| Borderline forms |
Acute disseminated encephalomyelitis · Balo concentric sclerosis · Devic's disease · Guillain-Barré syndrome · Marburg multiple sclerosis · Schilder's disease |
| Other |
List of people with multiple sclerosis · Multiple Sclerosis organizations |
| This page uses Creative Commons Licensed content from Wikipedia (view authors). |