Assessment |
Biopsychology |
Comparative |
Cognitive |
Developmental |
Language |
Individual differences |
Personality |
Philosophy |
Social |
Methods |
Statistics |
Clinical |
Educational |
Industrial |
Professional items |
World psychology |
Clinical: Approaches · Group therapy · Techniques · Types of problem · Areas of specialism · Taxonomies · Therapeutic issues · Modes of delivery · Model translation project · Personal experiences ·
| Haemophilia | |
|---|---|
| Classification and external resources | |
| ICD-10 | D66-D68 |
| ICD-9 | 286 |
| OMIM | 306700 306900 264900 |
| DiseasesDB | 5555 5561 29376 |
| MedlinePlus | 000537 |
| eMedicine | med/3528 |
| MeSH | D025861 |
Deficiency in coagulation factor VIII is the most common cause of haemophilia.
Haemophilia (also spelled hemophilia in North America, from the Greek haima αἷμα 'blood' and philia φιλος 'friend'[1]) is a group of hereditary genetic disorders that impair the body's ability to control blood clotting or coagulation, which is used to stop bleeding when a blood vessel is broken. Haemophilia A (clotting factor VIII deficiency) is the most common form of the disorder, occurring at about 1 in 5,000–10,000 male births.[2] Haemophilia B (factor IX deficiency) occurs at about 1 in about 20,000–34,000 male births.
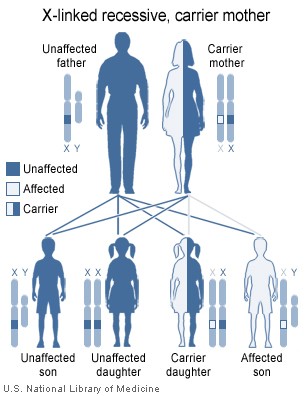
Similarly to most recessive sex-linked, X chromosome disorders, only males exhibit symptoms. This is due to the fact that females have two X chromosomes while males have only one, lacking a 'back up' copy for the defective gene the defective gene becomes manifest more easily in males. Because females have two X chromosomes and because haemophilia is rare, the chance of a female having two defective copies of the gene is very low, thus females are almost exclusively asymptomatic carriers of the disorder. Female carriers may inherit the defective gene from either their mother, father, or it may be a new mutation. Only under rare circumstances do females actually have haemophilia.
Haemophilia lowers blood plasma clotting factor levels of the coagulation factors needed for a normal clotting process. Thus when a blood vessel is injured, a temporary scab does form, but the missing coagulation factors prevent fibrin formation, which is necessary to maintain the blood clot. Thus a haemophiliac does not bleed more intensely than a normal person, but can bleed for a much longer amount of time. In severe haemophiliacs even a minor injury could result in blood loss lasting days, weeks, or not ever healing completely. In areas such as the brain or inside joints, this can be fatal or permanently debilitating.
Causes[]
- Haemophilia A is a recessive X-linked genetic disorder involving a lack of functional clotting Factor VIII and represents 90% of haemophilia cases.[3]
- Haemophilia B is a recessive X-linked genetic disorder involving a lack of functional clotting Factor IX. It is similar to but less common than haemophilia A.
- Haemophilia C is an autosomal genetic disorder (ie not X-linked) involving a lack of functional clotting Factor XI. Haemophilia C is not completely recessive: heterozygous individuals also show increased bleeding.[4]
Severity[]
There are numerous different mutations which cause each type of haemophilia. Due to differences in changes to the genes involved, patients with haemophilia often have some level of active clotting factor. Individuals with less than 1% active factor are classified as having severe haemophilia, those with 1-5% active factor have moderate haemophilia, and those with mild haemophilia have between 5-40% of normal levels of active clotting factor.[5]
Symptoms[]
Characteristic symptoms vary with severity. In general symptoms are internal or external bleeding episodes, which are called "bleeds".[6][7] Patients with more severe hemophilia suffer more severe and more frequent bleeds. While patients with mild haemophilia typically suffer more minor symptoms except after surgery or serious trauma. Moderate haemophiliacs have variable symptoms which manifest along a spectrum between severe and mild forms.
Prolonged bleeding and re-bleeding are the diagnostic symptoms of haemophilia. Internal bleeding is common in people with severe haemophilia and some individuals with moderate haemophilia. The most characteristic type of internal bleed is a joint bleed where blood enters into the joint spaces.[5] This is most common with severe haemophiliacs and can occur spontaneously (without evident trauma). If not treated promptly, joint bleeds can lead to permanent joint damage and disfigurement.[5] Bleeding into soft tissues such as muscles and subcutaneous tissues is less severe but can lead to damage and requires treatment.
Children with mild to moderate haemophilia may not have any signs or symptoms at birth especially if they do not undergo circumcision. Their first symptoms are often frequent and large bruises and hematomas from frequent bumps and falls as they learn to walk. Swelling and bruising from bleeding in the joints, soft tissue, and muscles may also occur. Children with mild haemophilia may not have noticeable symptoms for many years. Often, the first sign in very mild haemophiliacs is heavy bleeding from a dental procedure, an accident, or surgery. Females who are carriers usually have enough clotting factors from their one normal gene to prevent serious bleeding problems, though some may present as mild haemophiliacs.
Complications[]
Severe complications are much more common in severe and moderate haemophiliacs. Complications may be both directly from the disease or from its treatment:[8]
- Deep internal bleeding, e.g. deep-muscle bleeding, leading to swelling, numbness or pain of a limb.
- Joint damage, potentially with severe pain and even destruction of the joint and development of arthritis.
- Transfusion transmitted infection from blood transfusions that are given as treatment.
- Adverse reactions to clotting factor treatment, including the development of an immune inhibitor which renders factor replacement less effective.
- Intracranial hemorrhage, is a serious medical emergency cause by the buildup of pressure inside the skull. It can cause disorientation, nausea, loss of consciousness, brain damage, and death.
Treatment[]
Though there is no cure for haemophilia, it can be controlled with regular infusions of the deficient clotting factor, i.e. factor VIII in haemophilia A or factor IX in haemophilia B. Factor replacement can be either isolated from human blood serum, recombinant, or a combination of the two. Some haemophiliacs develop antibodies (inhibitors) against the replacement factors given to them, so the amount of the factor has to be increased or non-human replacement products must be given, such as porcine factor VIII.
Commercially produced factor concentrates such as "Advate", a recombinant Factor VIII produced by Baxter International, come as a white powder in a vial which must be mixed with sterile water prior to intravenous injection.
If a patient becomes refractory to replacement coagulation factor as a result of circulating inhibitors, this may be partially overcome with recombinant human factor VII (NovoSeven), which is registered for this indication in many countries.
In early 2008, the US Food and Drug Administration (FDA) approved Xyntha (Wyeth) anti-haemophilic factor, genetically engineered from the genes of Chinese hamster ovary cells. Since 1993 (Dr. Mary Nugent) recombinant factor products (which are typically cultured in Chinese hamster ovary (CHO) tissue culture cells and involve little, if any human plasma products) have been available and have been widely used in wealthier western countries. While recombinant clotting factor products offer higher purity and safety, they are, like concentrate, extremely expensive, and not generally available in the developing world. In many cases, factor products of any sort are difficult to obtain in developing countries.
In Western countries, common standards of care fall into one of two categories: prophylaxis or on-demand. Prophylaxis involves the infusion of clotting factor on a regular schedule in order to keep clotting levels sufficiently high to prevent spontaneous bleeding episodes. On-demand treatment involves treating bleeding episodes once they arise. In 2007, a clinical trial was published in the New England Journal of Medicine comparing on-demand treatment of boys (< 30 months) with haemophilia A with prophylactic treatment (infusions of 25 IU/kg body weight of Factor VIII every other day) in respect to its effect on the prevention of joint-diseases. When the boys reached 6 years of age, 93% of those in the prophylaxis group and 55% of those in the episodic-therapy group had a normal index joint-structure on MRI.[9] Prophylactic treatment, however, resulted in average costs of $300,000 per year. The author of an editorial published in the same issue of the NEJM supports the idea that prophylactic treatment not only is more effective than on demand treatment but also suggests that starting after the first serious joint related hemorrhage may be more cost effective than waiting until the fixed age to begin.[10] This study resulted in the first (October 2008) FDA approval to label any Factor VIII product to be used as prophylactically.[11] As a result, the factor product used in the study (Bayer's Kognate) is now labeled for use to prevent bleeds, making it more likely that insurance carries in the US will reimburse consumers who are prescribed and use this product prophylactically. Despite Kognate only recently being "approved" for this use in the US, it and other factor products have been well studied and are often prescribed to treat Haemophilia prophylactically to prevent bleeds, especially joint bleeds.[12]
Preventive exercises[]
It is recommended that people affected with haemophilia do specific exercises to strengthen the joints, particularly the elbows, knees, and ankles.[13] Exercises include elements which increase flexibility, tone, and strength of muscles, increasing their ability to protect joints from damaging bleeds. These exercises are recommended after an internal bleed occurs and on a daily basis to strengthen the muscles and joints to prevent new bleeding problems. Many recommended exercises include standard sports warm-up and training exercises such as stretching of the calves, ankle circles, elbow flexions, and quadriceps sets.
Alternative and complementary treatments[]
While not a replacement for traditional treatments, preliminary scientific studies indicate that hypnosis and self-hypnosis can be effective at reducing bleeds and the severity of bleeds and thus the frequency of factor treatment.[14][15][16][17] Herbs which strengthen blood vessels and act as astringents may benefit patients with haemophilia, however there are no peer reviewed scientific studies to support these claims. Suggested herbs include: Bilberry (Vaccinium myrtillus), Grape seed extract (Vitis vinifera), Scotch broom (Cytisus scoparius), Stinging nettle (Urtica dioica), Witch hazel (Hamamelis virginiana), and yarrow (Achillea millefolium).[14]
Occurrence[]
Haemophilia is rare, with only about 1 instance in every 10,000 births (or 1 in 5,000 male births) for haemophilia A and 1 in 50,000 births for haemophilia B.[18] About 18,000 people in the United States have haemophilia. Each year in the US, about 400 babies are born with the disorder. Haemophilia usually occurs in males and less often in females.[19] It is estimated that about 2500 Canadians have haemophilia A, and about 500 Canadians have haemophilia B.[20]
Genetics[]
Females possess two X-chromosomes, males have one X and one Y chromosome. Since the mutations causing the disease are recessive, a woman carrying the defect on one of her X-chromosomes may not be affected by it, as the equivalent allele on her other chromosome should express itself to produce the necessary clotting factors. However, the Y-chromosome in men has no gene for factors VIII or IX. If the genes responsible for production of factor VIII or factor IX present on a male's X-chromosome are deficient there is no equivalent on the Y-chromosome, so the deficient gene is not masked by the dominant allele and he will develop the illness.
Since a male receives his single X-chromosome from his mother, the son of a healthy female silently carrying the deficient gene will have a 50% chance of inheriting that gene from her and with it the disease; and if his mother is affected with haemophilia, he will have a 100% chance of being a haemophiliac. In contrast, for a female to inherit the disease, she must receive two deficient X-chromosomes, one from her mother and the other from her father (who must therefore be a haemophiliac himself). Hence haemophilia is far more common among males than females. However, it is possible for female carriers to become mild haemophiliacs due to lyonisation (inactivation) of the X chromosomes. Haemophiliac daughters are more common than they once were, as improved treatments for the disease have allowed more haemophiliac males to survive to adulthood and become parents. Adult females may experience menorrhagia (heavy periods) due to the bleeding tendency. The pattern of inheritance is criss-cross type. This type of pattern is also seen in colour blindness.
A mother who is a carrier has a 50% chance of passing the faulty X chromosome to her daughter, while an affected father will always pass on the affected gene to his daughters. A son cannot inherit the defective gene from his father.
Genetic testing and genetic counselling is recommended for families with haemophilia. Prenatal testing, such as amniocentesis, is available to pregnant women who may be carriers of the condition.
As with all genetic disorders, it is of course also possible for a human to acquire it spontaneously through mutation, rather than inheriting it, because of a new mutation in one of their parents' gametes. Spontaneous mutations account for about 33% of all cases of haemophilia A. About 30% of cases of haemophilia B are the result of a spontaneous gene mutation.
Probability[]
If a female gives birth to a haemophiliac child, either the female is a carrier for the disease or the haemophilia was the result of a spontaneous mutation. Until modern direct DNA testing, however, it was impossible to determine if a female with only healthy children was a carrier or not. Generally, the more healthy sons she bore, the higher the probability that she was not a carrier.
If a male is afflicted with the disease and has children with a female who is not even a carrier, his daughters will be carriers of haemophilia. His sons, however, will not be affected with the disease. The disease is X-linked and the father cannot pass haemophilia through the Y chromosome. Males with the disorder are then no more likely to pass on the gene to their children than carrier females, though all daughters they sire will be carriers and all sons they father will not have haemophilia (unless the mother is a carrier).
History[]
Queen Victoria passed haemophilia on to many of her descendants.
Scientific discovery[]
In 1803, Dr. John Conrad Otto, a Philadelphian physician, wrote an account about "a hemorrhagic disposition existing in certain families." He recognized that the disorder was hereditary and that it affected males and rarely females. He was able to trace the disease back to a woman who settled near Plymouth in 1720. The first usage of the term "haemophilia" appears in a description of the condition written by Hopff at the University of Zurich in 1828.[21] In 1937, Patek and Taylor, two doctors from Harvard, discovered anti-hemophilic globulin. Pavlosky, a doctor from Buenos Aires, found haemophilia A and haemophilia B to be separate diseases by doing a lab test. This test was done by transferring the blood of one haemophiliac to another haemophiliac. The fact that this corrected the clotting problem showed that there was more than one form of haemophilia.
European royalty[]
Haemophilia has featured prominently in European royalty and thus is sometimes known as "the royal disease". Queen Victoria passed the mutation to her son Leopold and, through several of her daughters, to various royals across the continent, including the royal families of Spain, Germany, and Russia. In Russia, Tsarevich Alexei Nikolaevich, son of Nicholas II, was a descendant of Queen Victoria through his mother Empress Alexandra and suffered from haemophilia. It was claimed that Rasputin was successful at treating the Tsarevich's haemophilia. At the time, a common treatment administered by professional doctors was to use aspirin, which worsened rather than lessened the problem. It is believed that, by simply advising against the medical treatment, Rasputin could bring visible and significant improvement to the condition of Alexei. In Spain, Queen Victoria's youngest daughter, Princess Beatrice, had a daughter Victoria Eugenie of Battenberg, who later became Queen of Spain. Two of her sons were haemophiliacs and both died from minor car accidents: Her eldest son, Prince Alfonso of Spain, Prince of Asturias, died at the age 31 from internal bleeding after his car hit a telephone booth. Her youngest son, Infante Gonzalo, died at age 19 from abdominal bleeding following a minor car accident where he and his sister hit a wall avoiding a cyclist. Neither appeared injured or sought immediate medical care and Gonzalo died two days later from internal bleeding.
Blood contamination issues[]
Prior to 1985, there were no laws enacted within the U.S. to screen blood. As a result, many haemophilia patients who received untested and unscreened clotting factor prior to 1992 were at an extreme risk for contracting HIV and hepatitis C via these blood products. It is estimated that more than 50% of the haemophilia population, over 10,000 people, contracted HIV from the tainted blood supply in the United States alone.[22]
As a direct result of the contamination of the blood supply in the late 1970s and early/mid 1980s with viruses such as hepatitis and HIV, new methods were developed in the production of clotting factor products. The initial response was to heat-treat (pasteurize) plasma-derived factor concentrate, followed by the development of monoclonal factor concentrates, which use a combination of heat treatment and affinity chromatography to inactivate any viral agents in the pooled plasma from which the factor concentrate is derived. The Lindsay Tribunal in Ireland investigated, among other things, the slow adoption of the new methods.
Differential diagnosis[]
Haemophilia A can be mimicked by von Willebrand disease
- von Willebrand Disease type 2A, where decreased levels of von Willebrand Factor can lead to premature proteolysis of Factor VIII. In contrast to haemophilia, vWD type 2A is inherited in an autosomal dominant fashion.
- von Willebrand Disease type 2N, where von Willebrand Factor cannot bind Factor VIII, autosomal recessive inheritance. (ie; both parents need to give the child a copy of the gene).[23]
- von Willebrand Disease type 3, where lack of von Willebrand Factor causes premature proteolysis of Factor VIII. In contrast to haemophilia, vWD type 3 is inherited in an autosomal recessive fashion.
See also[]
- Coagulopathy
- Contaminated haemophilia blood products
- List of haemophilia organizations
- Purpura secondary to clotting disorders
External links[]
- Hemophilia at the Open Directory Project
- Hemophilia.ca, Hemophilia A & B information, Canadian Hemophilia Society
- Hemophilia.org, Types of Bleeding Disorders], UK Haemophilia Society
- WFH.org, Online Hemophilia Publications Library: World Hemophilia Federation
- Haemophilia.org.uk, An Introduction to Haemophilia, UK Haemophilia Society
References[]
- ↑ Douglas Harper. Online Etymology Dictionary. URL accessed on 2007-10-10.
- ↑ Hemophilia B. URL accessed on 2007-11-21.
- ↑ www.wrongdianosis.com/h/hemophilia/stats.htm#medical_stats
- ↑ Prasad Mathew, MBBS, DCH, eMedicine - Hemophilia C
- ↑ 5.0 5.1 5.2 Hemophilia overview Emedicine.medscape.com, Dimitrios P Agaliotis, Robert A Zaiden, and Saduman Ozturk. Jan. 2, 2008.
- ↑ Types of Bleeds National Hemophilia Federation.
- ↑ Key facts: what is haemophilia? The Haemophilia Society.
- ↑ Hemophilia Complications By Mayo Clinic Staff. May 16, 2009
- ↑ Manco-Johnson MJ, Abshire TC, Shapiro AD, et al. (2007). Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N. Engl. J. Med. 357 (6): 535–44.
- ↑ Roosendaal G, Lafeber F (2007). Prophylactic treatment for prevention of joint disease in hemophilia—cost versus benefit. N. Engl. J. Med. 357 (6): 603–5.
- ↑ Kognate Product Approval Information USDA Center for Biologics Evaluation and Research.
- ↑ Hayes, P. 2009. FDA Approves Kognate For Prophylaxis. Hemaware: the bleeding disorder's magazine. Hemophilia Foundation. March/April 2009. Vol 14, Issue 2. p. 18.
- ↑ Mulder, K. 2006. Exercises for People with Hemophilia. World Federation of Hemophilia.
- ↑ 14.0 14.1 University of Maryland Medical Center Complementary medicines: Hemophilia
- ↑ New York Times, Science Watch; Hypnosis for Hemophiliacs May 6, 1986.
- ↑ American Society of Clinical Hypnosis. Asch.net, Information for the General Public
- ↑ David Spiegel 1994. Dissociation: Culture, Mind, and Body. American Psychiatric Pub. ISBN 0880485574, 9780880485579
- ↑ World Federation of Hemophilia Frequently Asked Questions About Hemophilia
- ↑ U.S. National Library of Medicine. URL accessed on 2007-12-02.
- ↑ Canadian Hemophilia Society FAQ
- ↑ The History of hemophilia. URL accessed on 2009-06-05.
- ↑ In re Rhone-Poulenc Rorer Inc., 51 F.3d 1293, 1296 (7th Cir. 1995), Projectposner.org, Retrieved 2008-01-28
- ↑ Von Willebrand disease#Tpy 2N
Template:Diseases of RBCs and megakaryocytes
| This page uses Creative Commons Licensed content from Wikipedia (view authors). |